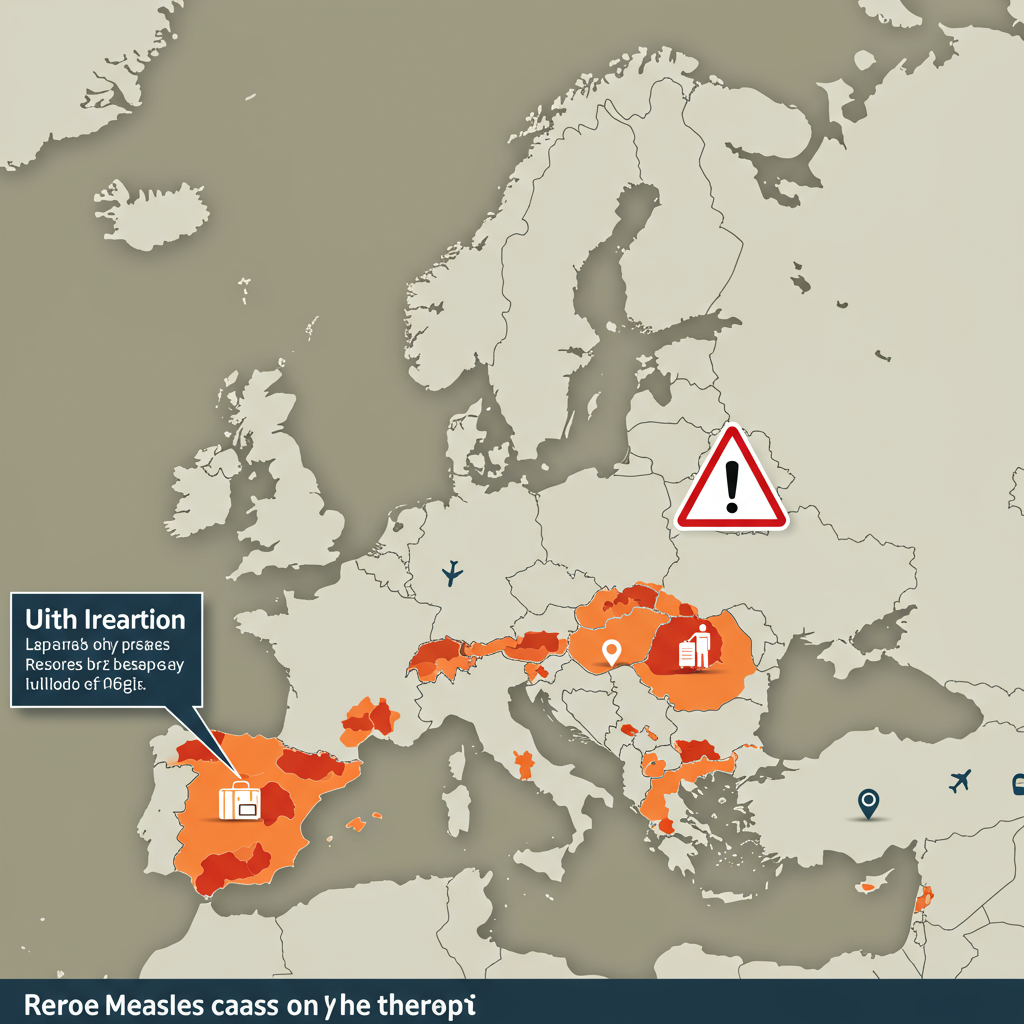
A significant global health dispute is unfolding as Guinea-Bissau, a West African nation, has decisively suspended a US-funded hepatitis B vaccine study. This pivotal move, confirmed by local officials, underscores profound concerns about research ethics, national sovereignty, and the appropriate conduct of clinical trials in vulnerable populations. The decision comes amidst sharp disagreements between African health leaders and US authorities, sparking an international dialogue on power dynamics in scientific research.
This contentious study, intended to investigate the “general health effects” of the hepatitis B vaccine at birth, received a substantial $1.6 million grant from the US Centers for Disease Control and Prevention (CDC). It was to be led by Danish researchers from the Bandim Health Project at the University of Southern Denmark. However, the trial design immediately drew widespread condemnation from public health experts globally, who deemed it “unethical and unnecessary.”
Guinea-Bissau Halts Study Amidst Ethical Storm
On Thursday, January 23, 2026, Quinhin Nantote, Guinea-Bissau’s recently appointed Minister of Health, unequivocally confirmed the study’s “cancellation or suspension.” He cited inadequate scientific review and a lack of proper coordination with national health authorities as key reasons for the decision. This announcement followed a November coup in the country, which brought new leadership into power and perhaps a renewed resolve for national control over critical health initiatives.
The heart of the ethical debate lies in the study’s proposed design. Researchers planned to enroll 14,000 infants, dividing them into two groups. One group of 7,000 newborns would receive the hepatitis B vaccine at birth, along with routine tuberculosis and polio shots. Crucially, the other 7,000 infants would not receive the hepatitis B vaccine until six weeks of age, or even later, delaying a critical intervention in a region with high disease prevalence.
Conflicting Stances: Africa CDC vs. US HHS
The suspension by Guinea-Bissau officials directly contradicted earlier assertions from the US Department of Health and Human Services (HHS). Initially, HHS spokesperson Andrew Nixon insisted the trial would “proceed as planned,” even accusing the Africa Centres for Disease Control and Prevention (Africa CDC) of a “public-relations campaign” and labeling it a “powerless, fake organization.” He offered no proof for these serious claims.
However, the tide turned when Africa CDC Director-General Jean Kaseya strongly refuted these allegations. Kaseya emphasized the Africa CDC’s crucial role in continental health responses and its mandate from 55 African heads of state. He stated that the decision rests solely with Guinea-Bissau, affirming the principle of national sovereignty. Following mounting pressure, HHS later revised its stance, confirming that the trial was indeed “paused pending further evaluation” but still avoiding direct answers on the ethical concerns or its earlier disparaging remarks about the Africa CDC.
Unpacking the Ethical Dilemmas and WHO Guidelines
The ethical outcry against the Guinea-Bissau vaccine study is rooted in widely accepted global health standards. The World Health Organization (WHO) unequivocally recommends that all newborns receive a dose of the hepatitis B vaccine within 24 hours of birth. This early intervention is critical to prevent mother-to-child transmission, which can lead to chronic infection, severe liver disease, and premature death, especially in endemic areas.
Guinea-Bissau faces a severe hepatitis B burden, with nearly one in five adults and about 11% of young children already infected. Delaying vaccination for half of the study’s infants, as proposed, would expose them to unnecessary risk, contravening the established standard of care. Dr. Abdulhammad Babatunde, a Nigerian global health researcher, starkly criticized the design, drawing parallels to historical ethical failures like the infamous Tuskegee study. He argued that ethical research demands control groups receive at least the standard of care, while intervention groups potentially receive improved care.
US Policy Shift and its Global Implications
Adding another layer of complexity to the controversy is a recent shift in US vaccine policy. For over three decades, the US had aligned with WHO recommendations, administering the hepatitis B vaccine to all newborns. However, in December of the previous year, the CDC’s Advisory Committee on Immunization Practices (ACIP), reportedly influenced by vaccine-skeptic figures within the administration, voted to overturn this long-standing policy.
This domestic policy change for the US is seen by many critics as a potential catalyst for the controversial Guinea-Bissau vaccine study. The timing of the CDC’s $1.6 million grant—less than two weeks after the ACIP vote—raised significant red flags. Experts, including virologist Angela Rasmussen, suggested concerns of “cronyism” and “bad science,” implying the researchers were hand-picked due to their known skepticism regarding vaccine safety. The study’s objective to investigate “overall health outcomes” rather than directly assessing vaccine efficacy against hepatitis B further fueled suspicions about its true scientific intent.
The Role of National Sovereignty and African Leadership
The Guinea-Bissau government’s firm stance reinforces the critical principle of national sovereignty in international research. Africa CDC Director-General Jean Kaseya reiterated that authorization for clinical trials must originate from the host countries themselves. He outlined specific requirements: written authorization from the National Medicine Regulatory Authority, approval from the National Ethical Committee, a local institutional review board, and explicit government clearance from the Ministry of Health.
Kaseya emphasized that African health priorities should drive research, not merely “the curiosity of the funders.” The Africa CDC has offered technical support to Guinea-Bissau to aid in reviewing the study, inviting officials from Denmark and the US to participate. This proactive approach by Africa CDC highlights a growing assertiveness from African institutions in safeguarding their populations and directing research agendas to genuinely address local health challenges.
Broader Concerns: Ethics Committee Approval and Scientific Integrity
Further scrutiny revealed issues with the study’s initial approval process. An early version was approved by Guinea-Bissau’s six-person ethics committee (CNEPS) in November. However, the interim director of CNEPS stated that this approval did not explicitly mention withholding vaccines from newborns, which became the central ethical concern. Minister Nantote expressed that CNEPS might not have adequately addressed these critical issues.
Moreover, the Danish researchers reportedly made updates to the study design that were not subsequently approved by CNEPS. Troublingly, they also did not appear to seek approval from ethics boards in Denmark or the US, a clear violation of the Helsinki Declaration, which mandates ethical committee approval in both sponsoring and host countries.
Beyond the immediate ethical lapses, questions about the scientific integrity of the Bandim Health Project researchers have also surfaced. A review in the journal Vaccine indicated that the team, particularly Dr. Christine Stabell Benn, had a history of “systematically over-interpreting” findings, with conclusions often unsupported by data. This academic scrutiny, combined with the non-competitive nature of the CDC grant, intensifies concerns about the motivations and scientific rigor behind the proposed Guinea-Bissau vaccine study.
Frequently Asked Questions
What are the main ethical concerns surrounding the Guinea-Bissau vaccine study?
The primary ethical concern stems from the study’s design, which proposed withholding the hepatitis B vaccine from 7,000 newborns until six weeks of age or later, despite the World Health Organization (WHO) recommending vaccination within 24 hours of birth. Given the high prevalence of hepatitis B in Guinea-Bissau, critics argue this design exposes vulnerable infants to unnecessary infection risks, deviating from the established standard of care. This raises parallels to historical unethical research practices, such as the Tuskegee study, by intentionally delaying a known protective intervention.
How has the US Department of Health and Human Services (HHS) responded to the study’s suspension?
Initially, the US Department of Health and Human Services (HHS) insisted the Guinea-Bissau vaccine study would proceed as planned, dismissing claims of its suspension and disparaging the Africa Centres for Disease Control and Prevention (Africa CDC). However, after strong pushback from Africa CDC and Guinea-Bissau officials affirming national sovereignty, HHS revised its statement, confirming the trial was “paused pending further evaluation.” Despite this acknowledgement, HHS has largely refrained from addressing the specific ethical concerns raised or retracting its earlier criticisms of the Africa CDC, leading to ongoing international scrutiny.
Why is national sovereignty a crucial factor in international clinical trials like the Guinea-Bissau hepatitis B study?
National sovereignty is paramount in international clinical trials because it ensures that host countries have the ultimate authority and responsibility over research conducted within their borders. This principle protects vulnerable populations from externally imposed studies that may not align with local health priorities or ethical standards, preventing potential exploitation. For the Guinea-Bissau vaccine study, the country’s assertion of sovereignty meant its Ministry of Health could halt a study deemed ethically questionable, emphasizing that local approval, ethical review, and genuine benefit to the local population must precede any foreign-funded research.
Moving Forward: A Call for Global Health Equity
The suspension of the Guinea-Bissau vaccine study serves as a stark reminder of the complexities and ethical imperatives in global health research. It highlights the critical need for genuine partnership, respect for national sovereignty, and unwavering commitment to ethical standards that prioritize the well-being of all participants. As discussions continue, the international community watches to see if this incident will pave the way for more equitable and ethically sound research practices that truly serve the needs of the populations they aim to help.