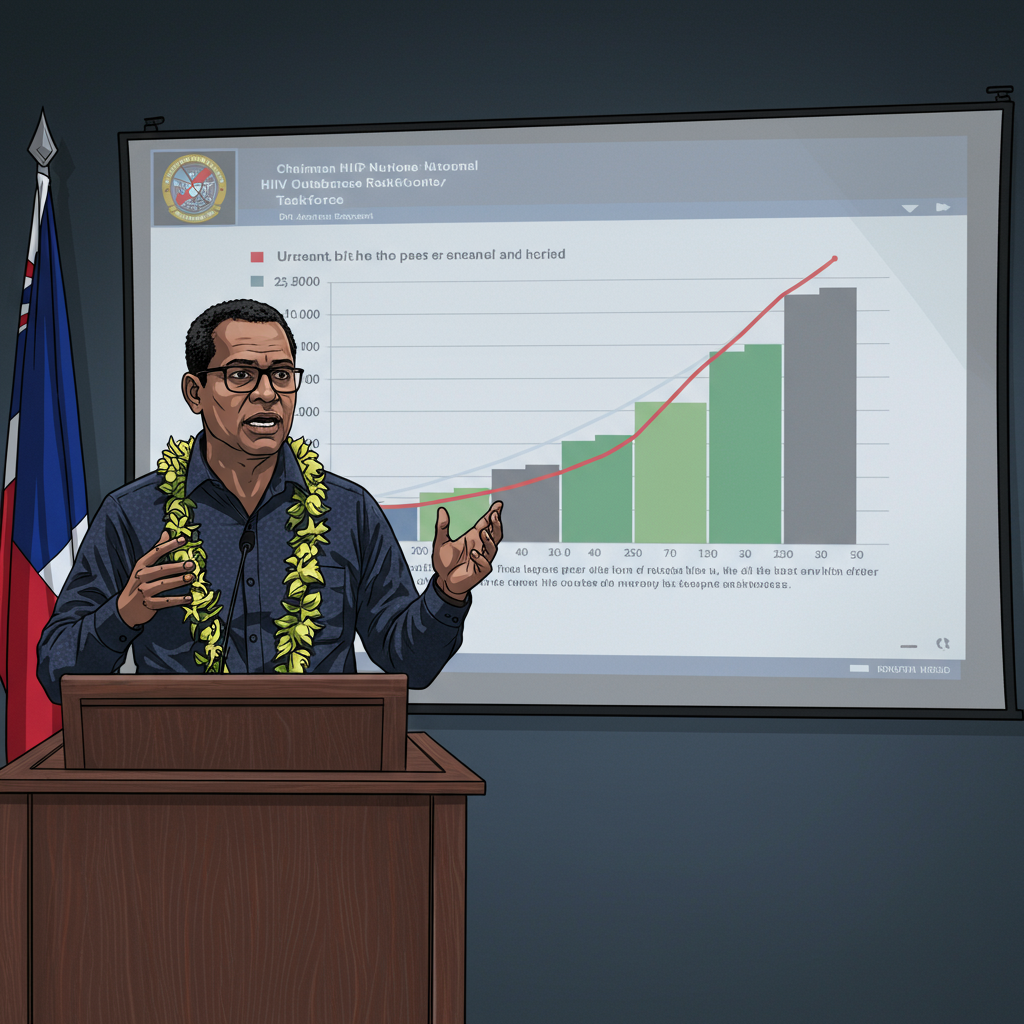
Fiji is grappling with a rapidly escalating HIV epidemic, now identified as the fastest-growing globally. Urgent warnings from Dr. Jason Mitchell, Chairman of the Fiji National HIV Outbreak Cluster Response Taskforce, highlight an alarming ten-fold increase in new infections since 2014, with projections suggesting nearly 25,000 HIV cases within the next four years if immediate action isn’t taken. This critical public health challenge is primarily driven by a surge in intravenous drug use, particularly impacting adolescents and disproportionately affecting the iTaukei community. The clock is truly ticking for Fiji.
Fiji’s Alarming HIV Surge: A Global Epicenter
A recent UNAIDS report, “2025 Global AIDS Update, AIDS, Crisis and the Power to Transform,” casts a stark light on Fiji’s HIV situation. The data reveals a staggering ten-fold increase in new HIV infections across Fiji since 2014. This dramatic rise has propelled the nation to an unenviable position, with Dr. Jason Mitchell confirming that Fiji currently has the world’s fastest-growing HIV epidemic. The numbers paint a grim picture, underscoring a public health crisis that demands immediate and comprehensive intervention.
The sheer scale of the challenge is underscored by recent statistics. Between January and December 2024, Fiji recorded a concerning total of 1,583 new HIV diagnoses. This rapid accumulation of new cases is not merely a statistical anomaly; it represents a profound threat to public health and societal well-being. Dr. Mitchell’s stark warning of potentially 25,000 HIV cases in the next four years serves as a powerful call to action, emphasizing the dire consequences of inaction.
Intravenous Drug Use: The Primary Driver of New Infections
Crucially, the driving force behind this unprecedented surge in Fiji HIV infections has been clearly identified: intravenous drug use. Dr. Mitchell explicitly stated that the significant increase is not a result of sexual transmission. Instead, it is almost entirely attributable to high-risk practices associated with injecting drugs. This shift in transmission dynamics presents a unique challenge for public health officials, requiring specialized prevention strategies.
This epidemic’s trajectory is particularly concerning among vulnerable populations. The prevalence of injectable drug use has altered the demographic landscape of new HIV cases. Understanding the nuances of this transmission pathway is vital for crafting effective public health responses.
Vulnerable Youth at Unprecedented Risk
One of the most distressing statistics emerging from this crisis relates to Fiji’s youth. Over the past three years, there has been a staggering 45-fold increase in HIV infections among adolescents aged 10 to 19. This dramatic escalation within such a young age group is profoundly troubling. Dr. Mitchell firmly reiterated that this sharp rise among adolescents is directly linked to intravenous drug use, not sexual transmission.
The vulnerability of this age group underscores the urgent need for targeted harm reduction programs and education initiatives. These programs must be designed to reach young people engaged in high-risk behaviors, providing them with critical information and support to prevent further transmission. Addressing the root causes of drug use among youth is paramount to protecting the next generation from the devastating impact of HIV.
Clinical Manifestations and Opportunistic Infections
Beyond the raw statistics, the worsening Fiji HIV crisis is also evident in clinical settings. Doctors across Fiji’s hospitals are increasingly observing opportunistic infections. These are infections that typically do not affect individuals with healthy immune systems but commonly emerge in those with compromised immunity, a hallmark of advanced HIV. The growing presence of these unusual infections signifies that the virus is spreading, leading to a rising number of individuals with weakened immune responses within the population.
This clinical evidence provides tangible proof of the epidemic’s expanding footprint, moving beyond mere numbers to manifest in direct patient care. The strain on healthcare resources, as well as the long-term health implications for affected individuals, are significant concerns. Without effective intervention, this trend of increasing infections and associated health complications is projected to continue, according to Dr. Mitchell’s assessment of current patterns.
Disproportionate Impact on the iTaukei Community
A critical aspect of Fiji’s HIV epidemic is its uneven impact across demographic groups. Community-based testing efforts reveal that a disproportionate number of new HIV positive diagnoses are among the iTaukei population. Specifically, out of the 1,583 new HIV diagnoses recorded between January and December 2024, a staggering 90.3 percent (1,430 individuals) were from the iTaukei community. Dr. Mitchell noted that many individuals identified within key population groups engaged in high-risk behaviors belong to this indigenous community.
However, a significant knowledge gap exists regarding the underlying reasons for this disparity. There is currently no specific data or comprehensive research available to fully explain why the iTaukei population appears to be more affected by HIV compared to other groups in Fiji. This lack of detailed understanding presents a major challenge for designing culturally sensitive and effective public health campaigns. Addressing this requires focused research to uncover the socio-economic, cultural, and systemic factors contributing to this disproportionate impact, ensuring that future interventions are both equitable and effective.
Strategic Interventions and Tailored Messaging
In response to this multifaceted public health emergency, Dr. Mitchell emphasized the critical need for highly targeted approaches to combat the HIV crisis in Fiji. An effective HIV response necessitates developing and delivering messages specifically tailored to groups with identified risk factors, such as those involved in intravenous drug use or within the disproportionately affected iTaukei community.
The aim is to provide these communities with precise, relevant, and accessible information. This includes educating individuals on how their specific practices could contribute to the transmission of HIV and other blood-borne viruses. Empowering communities with accurate knowledge is crucial for enabling them to make informed decisions that mitigate risks and protect their health. These interventions involve not just medical treatment but also community outreach, education, and social support structures.
The Urgent Call to Action
The current trajectory of HIV infections in Fiji presents a grave warning. The stark figures – a ten-fold increase since 2014, a 45-fold surge among adolescents, and the projection of 25,000 cases in just four years – highlight the extreme urgency of the situation. Fiji’s position as the world’s fastest-growing HIV epidemic necessitates a unified and robust response from government, health organizations, community leaders, and individuals. Without immediate, comprehensive, and targeted interventions, the social and health costs to the nation will be immense and long-lasting. The time to act decisively against the Fiji HIV crisis is now.
Frequently Asked Questions
What is the current status of the HIV epidemic in Fiji?
Fiji is currently facing the world’s fastest-growing HIV epidemic, according to Dr. Jason Mitchell and a UNAIDS report. Since 2014, the number of new infections has risen ten-fold. Between January and December 2024 alone, 1,583 new HIV diagnoses were recorded. If current trends persist, Fiji could see nearly 25,000 HIV cases within the next four years, underscoring the severe and urgent nature of the public health crisis.
What are the primary factors driving the HIV crisis in Fiji?
The main driver of Fiji’s escalating HIV infections is intravenous (injectable) drug use. Dr. Jason Mitchell confirmed that this is the primary cause, not sexual transmission. A particularly alarming statistic highlights a 45-fold increase in HIV infections among adolescents aged 10 to 19 over the last three years, almost entirely attributed to high-risk practices associated with intravenous drug use within this young demographic.
What actions are being taken to address Fiji’s escalating HIV infections?
Dr. Jason Mitchell, as Chairman of the Fiji National HIV Outbreak Cluster Response Taskforce, emphasizes the need for highly targeted interventions. This includes developing specific messages tailored to groups with known risk factors, such as those involved in injectable drug use and the iTaukei community, which is disproportionately affected. The goal is to provide accurate information to help individuals understand how their practices can lead to HIV and other blood-borne viruses, enabling them to make informed decisions for prevention.