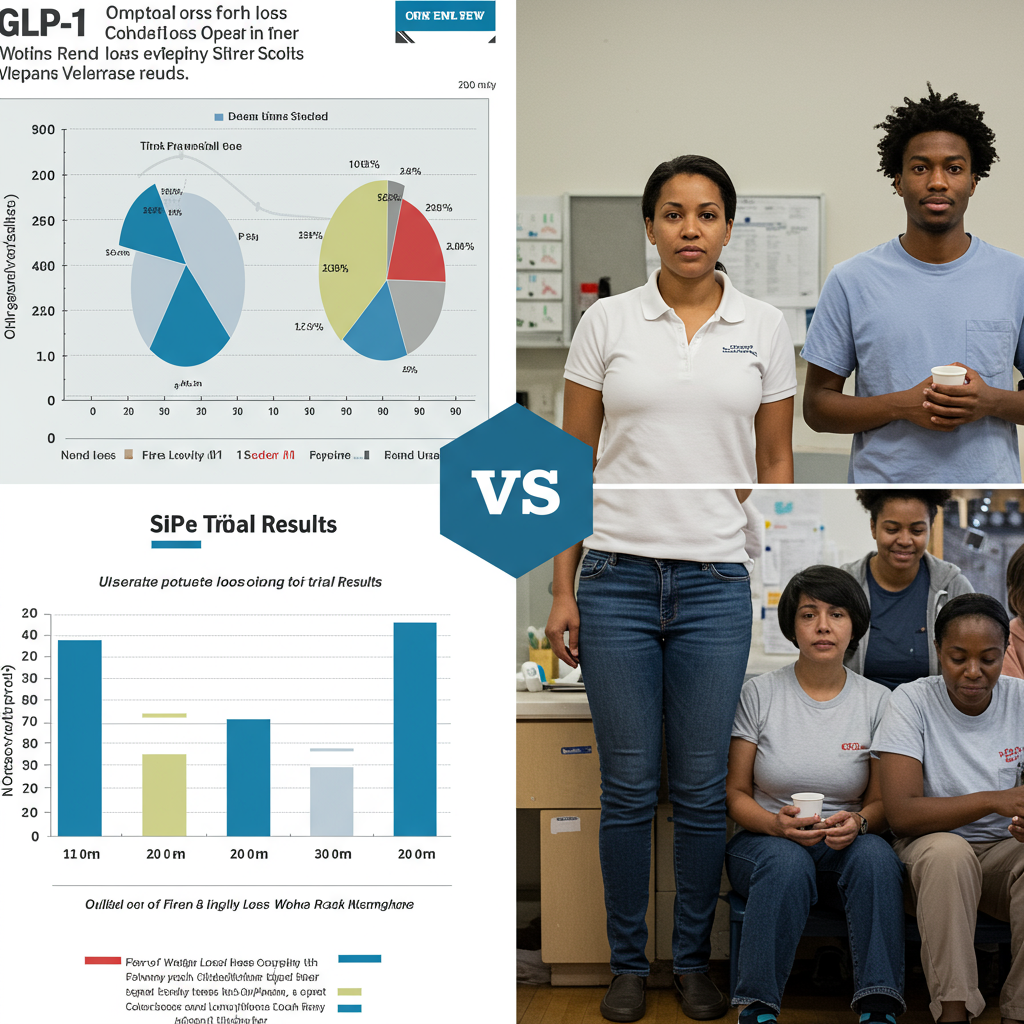
GLP-1 medications like Wegovy, Ozempic, Zepbound, and Mounjaro have revolutionized weight management, gaining immense popularity and now accounting for over 5% of adult prescriptions in the U.S. Their clinical trials showcased remarkable weight loss – semaglutide (the active ingredient in Ozempic/Wegovy) led to nearly 15% body weight reduction, while tirzepatide (Mounjaro/Zepbound) users saw over 20% loss in trials spanning over a year.
But are real-world patients experiencing the same dramatic results as trial participants? A new study analyzing observational data suggests that, on average, the answer is no.
Real-World Weight Loss Falls Short
According to research published June 10, 2025, in the journal Obesity, which examined data from nearly 7,900 real-world GLP-1 users (without type 2 diabetes) in Ohio and Florida, average weight loss over one year was notably less than seen in clinical trials.
Real-world semaglutide users saw an average weight reduction of 7.7%.
Real-world tirzepatide users averaged 12.4% body weight reduction.
While significant, these figures are substantially lower than the 14.9% and 20.9% averages reported in the pivotal clinical trials for these medications.
Why the Discrepancy? Key Factors Identified
Experts and the study authors point to critical differences between highly controlled clinical trial settings and the complexities of real-world treatment as the primary drivers behind this gap. Hamlet Gasoyan, PhD, MPH, a study author, explained, “In the real world, we observed weight reduction or weight loss was lower than what we [have] seen in randomized control trials,” attributing the difference largely to patients stopping treatment early and taking lower doses.
1. Early Treatment Discontinuation
A major factor identified is the high rate of patients discontinuing their GLP-1 medication prematurely. The study found that roughly half of the participants stopped taking their drug within the first year. The impact on weight loss was significant:
Patients who stopped within the first three months lost only about 3.6% of their body weight.
Those who continued for three to 12 months lost an average of 6.8%.
Achieving optimal weight loss with GLP-1s often requires patients to stay on the medication consistently to allow for gradual dose increases (titration), a process that can take around four months to reach the most effective maintenance levels. Prematurely stopping means many never experience the full therapeutic potential.
Why are patients stopping? Real-world challenges include:
Cost and Insurance: High out-of-pocket costs and difficulties obtaining insurance coverage or prior authorizations contribute to many prescriptions going unfilled or treatment being abandoned.
Side Effects: While generally well-tolerated, gastrointestinal side effects like nausea, vomiting, and diarrhea can be bothersome and lead patients to stop or reduce their dose.
Supply Shortages: Experts noted that supply issues during the study period were nearly three times higher than in clinical trials, forcing some patients to interrupt or discontinue treatment.
2. Lower Medication Dosages
Another significant reason for lower average weight loss in the real world is that many patients don’t reach the higher maintenance doses used in clinical trials. In the Obesity study, about 80% of participants were on lower doses (less than 1.7 mg semaglutide or less than 10 mg tirzepatide), often due to intolerance to side effects during the titration process.
However, the study provided a crucial insight: real-world patients who did manage to reach higher doses comparable to those in clinical trials achieved weight loss results much closer to the trial outcomes (13.7% with semaglutide and 18% with tirzepatide). This suggests that the medication can work nearly as effectively outside of trials if patients stay on treatment and tolerate dose escalation.
Real-World Findings Consistent with Broader Trends
Experts like Richard Siegel, MD, noted that these results are not surprising and align with patterns seen across weight management medications, where real-world effectiveness often trails clinical trial performance due to factors like adherence challenges. High discontinuation rates—estimated at 50-70% after one year for weight management therapies generally—underscore the difficulty patients face in maintaining long-term therapy.
Recognizing non-adherence as a significant barrier, pharmaceutical innovation is exploring solutions like long-acting implants designed for infrequent administration (potentially once or twice yearly) to ensure consistent drug delivery and potentially improve tolerability.
Even Modest Weight Loss Provides Big Benefits
Despite the difference compared to clinical trials, it’s critical to emphasize that the weight loss achieved by real-world GLP-1 users (7.7% and 12.4% on average) is still clinically meaningful. Experts highlight that even losing 5% of body weight can yield substantial health benefits, including improvements in blood pressure, cholesterol, and blood sugar levels, potentially preventing or reversing conditions like prediabetes. The Obesity* study itself found that higher dose use without discontinuation was linked to better glucose control in prediabetic patients.
Maximizing Your Results on GLP-1s
For individuals aiming to optimize their weight loss journey with GLP-1 medications, experts recommend several strategies:
- Commit to Long-Term Use: Understand that this is often a chronic treatment. Work with your healthcare provider to navigate potential challenges like side effects or access issues to stay on the medication consistently, aiming to reach and maintain the target dose if tolerated. Open discussions about costs and potential side effects early on can improve adherence.
- Titrate Dose as Tolerated: Gradual dose escalation, guided by your doctor, is key to reaching the effective therapeutic level while managing potential side effects. Patients on higher doses in the study were significantly more likely to achieve over 10% weight loss.
- Integrate Lifestyle Changes: Adopting healthy eating habits (focusing on nutrient-dense foods, eating slowly, avoiding greasy items) and regular physical activity are essential. These changes not only enhance the medication’s effects but are crucial for maintaining weight loss if medication is stopped, preventing weight regain.
- Seek Multidisciplinary Support: A care team including doctors, dietitians, and potentially support staff to navigate insurance and access can provide comprehensive assistance for both medication management and behavioral changes.
Looking Ahead: Beyond Weight Loss
The growing body of real-world data from millions of GLP-1 users is also revealing exciting potential applications beyond weight loss and diabetes. Research is exploring their effects on conditions like cardiovascular disease (already an approved indication for some), sleep apnea, addiction, Alzheimer’s disease risk, and even potential links to longevity, highlighting the broad impact these medications may have on public health.
In conclusion, while real-world average weight loss on GLP-1s may differ from the dramatic results seen in highly controlled clinical trials, the medication remains a powerful tool. Understanding the real-world challenges—primarily discontinuation and lower doses driven by access issues and side effects—is crucial. By focusing on consistent treatment, appropriate dosing with medical guidance, embracing lifestyle changes, and leveraging comprehensive support, individuals can significantly increase their chances of achieving meaningful and sustainable weight loss and metabolic health improvements.