The landscape of chronic skin conditions is shifting, with a notable increase in psoriasis diagnoses worldwide. This complex autoimmune disorder, characterized by rapid skin cell turnover, is becoming a more prevalent public health concern. Surprisingly, recent trends indicate that wealthier regions bear the heaviest burden of this global rise. Understanding this paradox is crucial for effective prevention, diagnosis, and management strategies. This article delves into the factors contributing to the escalating psoriasis rates and explores why developed nations appear to be at the forefront of this dermatological challenge.
The Global Psoriasis Landscape: A Growing Concern
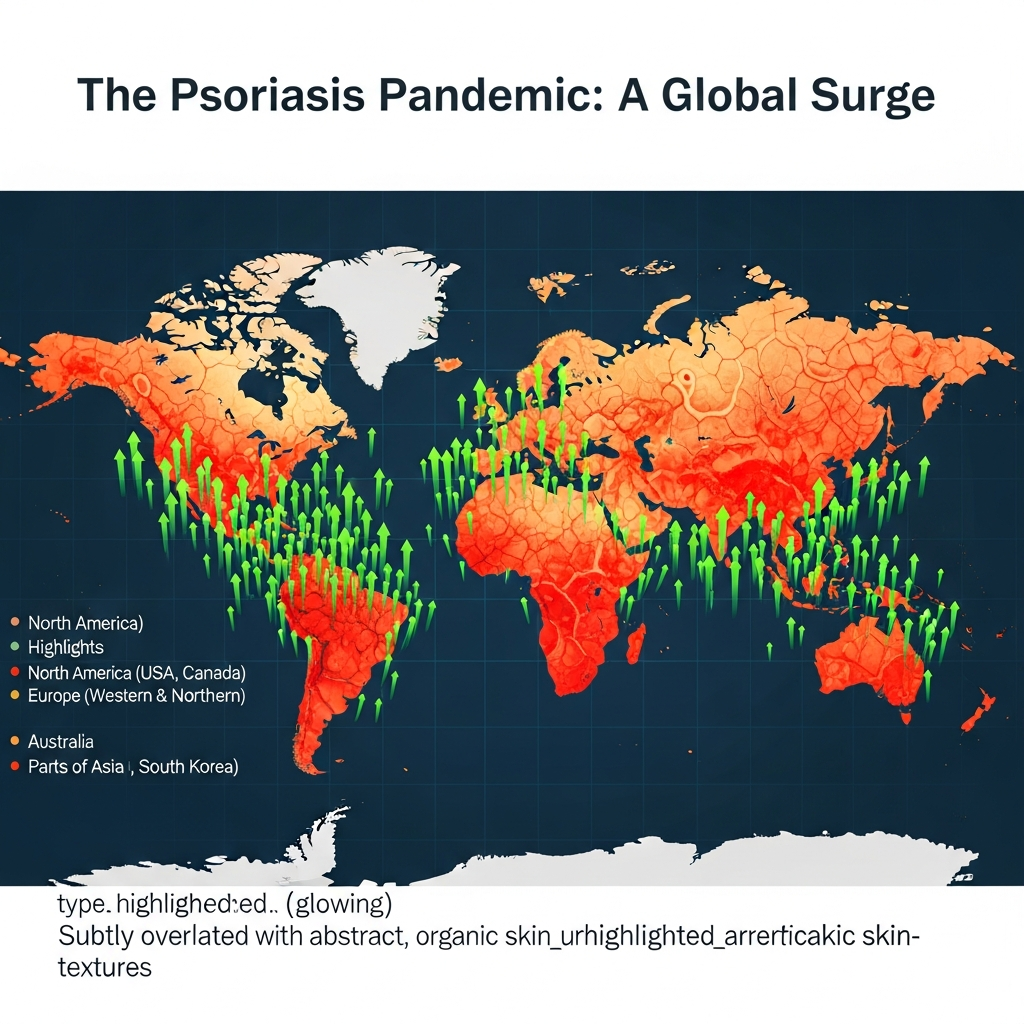
Psoriasis is far more than just a skin condition. It’s a chronic inflammatory disease impacting millions globally, often associated with significant physical and psychological distress. Historically, its prevalence varied widely across different populations. However, data now points to a consistent upward trajectory in psoriasis rates across continents. This surge isn’t merely an increase in awareness or diagnostic capabilities; it reflects a genuine expansion of the disease’s reach and impact.
This rise in global psoriasis prevalence highlights an urgent need for increased research, improved public health initiatives, and enhanced patient support. The condition can manifest in various forms, most commonly as plaque psoriasis, causing red, scaly patches on the skin. Yet, its systemic nature means it can also affect joints, leading to psoriatic arthritis, and is linked to other serious health issues.
Understanding Psoriasis: Beyond the Surface
Psoriasis occurs when the immune system mistakenly attacks healthy skin cells. This leads to an accelerated skin cell production cycle, forming thick, silvery scales and itchy, dry patches. While its exact cause remains unknown, it involves a complex interplay of genetic predisposition and environmental triggers. Living with psoriasis significantly impacts quality of life, affecting daily activities, self-esteem, and mental health. The visibility of lesions can lead to social stigma and isolation.
Effective management often requires a multi-faceted approach. This includes topical treatments, phototherapy, oral medications, and biologic injections. The goal is to reduce inflammation, slow skin cell growth, and manage symptoms. Early diagnosis and consistent treatment are vital to prevent progression and minimize complications.
Why Wealthier Regions Face a Higher Burden
The observation that wealthier regions experience a greater burden of rising psoriasis rates is particularly intriguing. This isn’t a simple correlation but suggests deeper societal, environmental, and healthcare-related factors at play. Several hypotheses attempt to explain this phenomenon, ranging from diagnostic advancements to lifestyle influences.
One significant factor is the improved access to healthcare and diagnostic services in developed nations. In regions with advanced medical infrastructure, individuals are more likely to seek medical attention for skin complaints. Dermatologists are more accessible, and diagnostic tools are readily available, leading to higher reported prevalence rates. This contrasts with developing regions where psoriasis might be underdiagnosed or misdiagnosed due to limited resources.
The Role of Lifestyle and Environment
Lifestyle choices prevalent in wealthier societies may also contribute to increased psoriasis risk. The “Western diet,” characterized by high intake of processed foods, red meat, and sugar, and low intake of fruits and vegetables, is increasingly linked to chronic inflammatory conditions. Obesity, a growing epidemic in many developed countries, is a known risk factor and can exacerbate existing psoriasis.
Furthermore, higher stress levels, common in fast-paced urban environments, can trigger or worsen psoriasis flare-ups. Smoking and excessive alcohol consumption, while global issues, might also contribute to higher incidence rates in populations where these habits are more widespread or have been historically prevalent. These environmental and lifestyle factors interact with genetic predispositions, creating a more fertile ground for the development and persistence of psoriasis.
Access to Healthcare and Diagnosis
While lifestyle factors play a role, the ability to actually identify and record cases cannot be overstated. In countries with robust healthcare systems, comprehensive screening and specialist referrals are more common. This means that mild or early-stage psoriasis, which might go unnoticed or untreated in regions with limited medical access, is more likely to be diagnosed and added to prevalence statistics in wealthier nations. This distinction between actual incidence and reported prevalence is crucial for understanding global health disparities. Enhanced medical literacy also contributes, as more people are aware of conditions like psoriasis and seek professional help.
The Ripple Effect: Beyond Skin Deep
The increasing psoriasis prevalence in wealthier regions extends beyond dermatological concerns. Psoriasis is a systemic inflammatory disease linked to a range of comorbidities. Patients with psoriasis, particularly severe forms, face a higher risk of developing psoriatic arthritis, cardiovascular diseases, metabolic syndrome, Crohn’s disease, and certain cancers. These associated conditions add to the overall health burden and healthcare costs, particularly in systems capable of diagnosing and managing them.
The mental health impact is also profound. Individuals with psoriasis often experience anxiety, depression, and social isolation due to the visible nature of their condition. The chronic pain and discomfort further contribute to a reduced quality of life. Addressing these multifaceted impacts requires an integrated approach that considers both physical and psychological well-being.
What This Means for Patients and Public Health
The rising global psoriasis rates, especially in developed nations, underscore the need for proactive public health strategies. For individuals, understanding the risk factors and recognizing early symptoms is key. Early diagnosis allows for prompt intervention, which can significantly improve outcomes and prevent disease progression. Lifestyle modifications, such as adopting a balanced diet, maintaining a healthy weight, managing stress, and avoiding smoking, can play a critical role in both preventing onset and managing existing symptoms.
From a public health perspective, there is a clear call for continued investment in research to unravel the complex etiologies of psoriasis. This includes exploring the interplay between genetics, environment, and lifestyle. Furthermore, awareness campaigns can reduce stigma and encourage individuals to seek help. Policy makers and healthcare providers must work together to ensure equitable access to effective treatments and support services, regardless of socioeconomic status or geographical location.
Empowering Patients: Knowledge and Action
Empowering individuals with knowledge about psoriasis is fundamental. Patients should be encouraged to work closely with their dermatologists to develop personalized treatment plans. Joining support groups or online communities can also provide invaluable emotional support and practical advice. Advocacy for better healthcare access and research funding is another powerful way to contribute to managing this growing global health challenge. By staying informed and proactive, individuals can navigate their journey with psoriasis more effectively.
Frequently Asked Questions
What factors contribute to the global rise in psoriasis rates?
The global rise in psoriasis rates is attributed to a combination of factors. These include improved diagnostic capabilities and healthcare access in developed regions, leading to higher reported cases. Lifestyle factors such as the “Western diet,” increased obesity, higher stress levels, and prevalent smoking and alcohol consumption in wealthier nations also play a significant role. Additionally, an aging population, where psoriasis may manifest or become more severe, contributes to the overall increase in prevalence.
Where can individuals find support and resources for managing psoriasis?
Individuals seeking support and resources for managing psoriasis should first consult a qualified dermatologist for an accurate diagnosis and personalized treatment plan. Beyond medical professionals, numerous patient advocacy organizations, such as the National Psoriasis Foundation (NPF) in the U.S. or Psoriasis Association in the UK, offer extensive resources, support groups, and educational materials. Online forums and communities also provide valuable peer support and practical advice for living with the condition.
Should lifestyle changes be a primary focus for someone diagnosed with psoriasis?
Yes, lifestyle changes can be a crucial primary focus for individuals diagnosed with psoriasis. While not a cure, adopting a healthy lifestyle can significantly impact disease management and overall well-being. This includes maintaining a balanced diet, managing a healthy weight, reducing stress through mindfulness or exercise, avoiding smoking, and limiting alcohol consumption. These changes can help reduce inflammation, minimize flare-ups, and potentially improve the effectiveness of medical treatments, making them a powerful complementary approach to clinical care.
Conclusion
The rising global psoriasis rates, particularly concentrated in wealthier regions, present a complex and evolving public health challenge. This trend highlights a critical interplay between genetic predispositions, environmental exposures, lifestyle choices, and the availability of advanced healthcare. As we continue to unravel the mysteries of this chronic autoimmune condition, it’s clear that a multifaceted approach is essential. This includes ongoing research into its causes, improved diagnostic tools, broader access to effective treatments, and robust public health campaigns focusing on prevention and awareness. By understanding the “why” behind these geographical disparities, we can better equip patients and healthcare systems to manage the growing burden of psoriasis worldwide, fostering better health outcomes and improving quality of life for those affected.