A perplexing and severe vomiting condition linked to long-term cannabis use, known as Cannabis Hyperemesis Syndrome (CHS), is now officially recognized by global health authorities. This pivotal step by the World Health Organization (WHO) and subsequent adoption by the Centers for Disease Control and Prevention (CDC) offers a new beacon of hope for thousands of sufferers. Previously misdiagnosed for years, CHS cases have surged dramatically across the U.S., prompting medical experts to highlight the critical need for awareness, accurate diagnosis, and effective intervention for this often debilitating and sometimes deadly syndrome.
Understanding Cannabis Hyperemesis Syndrome (CHS)
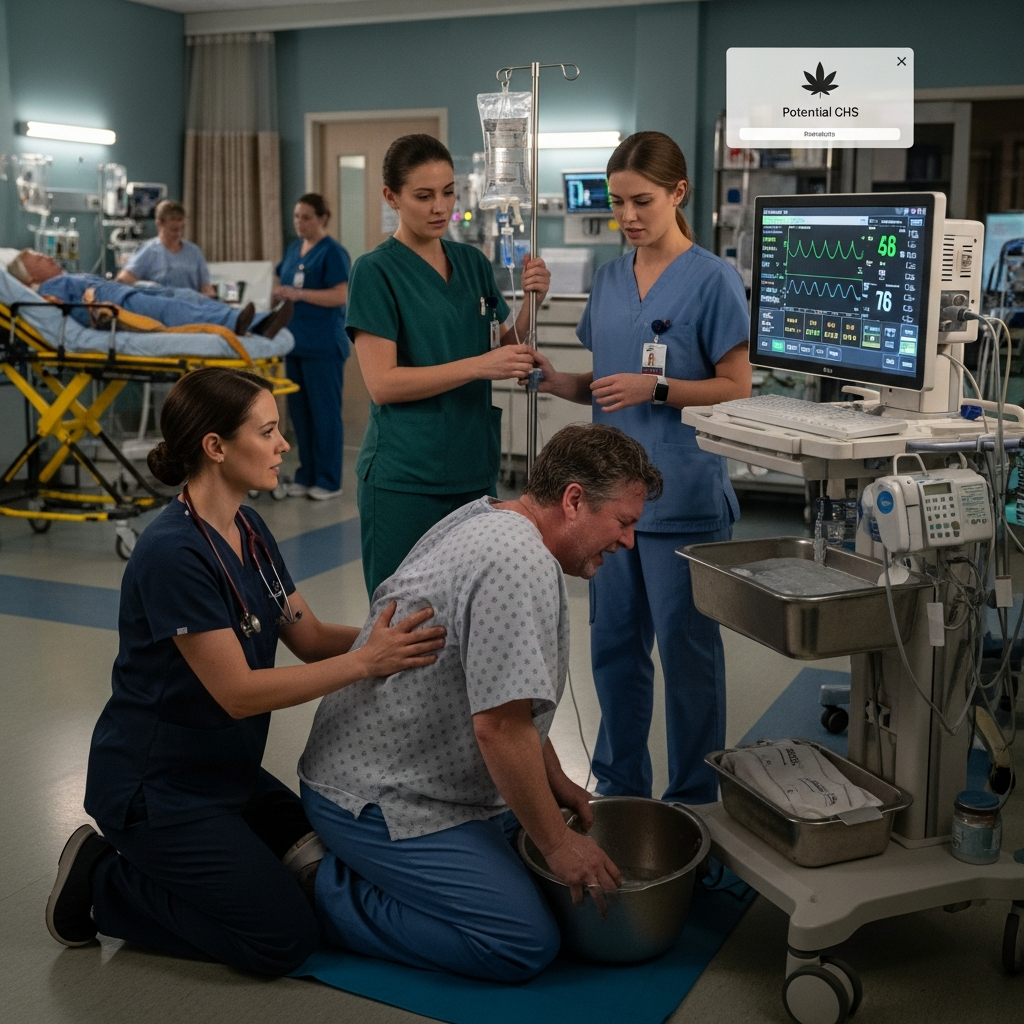
Cannabis Hyperemesis Syndrome is a debilitating condition affecting chronic cannabis users. It triggers intense, recurring episodes of nausea, severe vomiting, and significant abdominal pain. Patients often describe a horrifying symptom called “scromiting,” where extreme pain causes them to scream and vomit simultaneously. This syndrome can lead to dehydration, substantial weight loss, and in rare, severe instances, critical complications like kidney failure, seizures, and dangerous heart rhythm problems, sometimes even resulting in death.
The Challenge of Diagnosis and Misconceptions
For years, diagnosing CHS proved incredibly difficult. Its symptoms frequently mimic other common ailments such as food poisoning or the stomach flu. This similarity often left patients without answers for months, or even years, enduring countless emergency room visits and significant medical costs before receiving a correct diagnosis. Many doctors were simply unfamiliar with the syndrome. John Puls, a nationally certified addiction specialist, notes that a common misconception is that CHS isn’t a real condition at all. The new diagnostic code aims to correct this.
The Alarming Rise in CHS Cases and High-Potency Cannabis
The incidence of CHS has escalated dramatically, a trend health experts link directly to today’s prevalent high-potency cannabis products. A JAMA Network Open study published in November revealed a staggering 650% increase in emergency room visits for CHS between 2016 and the peak of the COVID-19 pandemic. These numbers have remained alarmingly high ever since, particularly among individuals aged 18 to 35. Researchers suggest that factors like increased isolation, heightened stress, and easier access to highly potent cannabis products contributed significantly to this surge.
The Potency Problem: A Key Driver?
The study also highlighted a profound shift in THC potency. Modern cannabis products frequently contain over 20% THC, a sharp contrast to the approximately 5% common in the 1990s. Some products even exceed 90% THC content. John Puls has observed an “alarming” increase in CHS, especially among adolescents and young adults who frequently use these high-potency products. He firmly believes that the elevated rates of CHS are unequivocally linked to this dramatic increase in THC concentration. This correlation is particularly concerning given that emergency department visits for CHS among adolescents in the U.S. jumped over tenfold from 2016 to 2023. Interestingly, the fastest year-over-year increases in adolescent cases occurred in states where casual cannabis use remains illegal, suggesting widespread access regardless of legal status.
Unraveling the Mystery: Theories Behind CHS
While the exact underlying cause of CHS remains unknown, the leading scientific theory points to the long-term overstimulation of the body’s endocannabinoid system. This system plays a crucial role in regulating various bodily functions, including nausea and vomiting. Paradoxically, while cannabis is often used to alleviate nausea (typically at much lower THC doses, under 5%), heavy, chronic use of high-THC products may disrupt this delicate balance. The overstimulation could trigger an opposite effect, leading to the severe vomiting episodes characteristic of CHS. It remains unclear why some chronic users develop the syndrome while others do not.
Finding Relief: Treatment and Recovery Pathways
The only confirmed “surefire cure” for Cannabis Hyperemesis Syndrome is the complete cessation of cannabis use. This can be a significant challenge due to the addictive nature of cannabis. Standard anti-nausea medications are generally ineffective against CHS. Instead, doctors often turn to stronger drugs or recommend capsaicin cream, which provides a warming sensation akin to the temporary relief many patients find in taking long, hot showers. This peculiar relief from hot showers is a telltale sign of CHS, though scientists still don’t fully understand why it works. Dr. Chris Buresh, an emergency medicine specialist, notes that this unique symptom can often “clinch the diagnosis.”
Breaking the Cycle of Relapse
The intermittent nature of CHS often complicates recovery. Sufferers may experience a severe episode, recover, and then mistakenly believe it was a fluke unrelated to their cannabis use. This can lead them to continue using cannabis, only to become violently sick again. Many individuals resist the CHS diagnosis, and even those who accept it often struggle to quit due to addiction. Experts warn that once someone has experienced CHS, they are much more likely to have recurring episodes, even with seemingly small amounts of cannabis.
The Significance of the WHO Diagnostic Code
The formal recognition of Cannabis Hyperemesis Syndrome by the WHO, with a dedicated diagnostic code, marks a monumental step forward. This update, effective October 1st and adopted by the CDC, empowers physicians nationwide to accurately identify, track, and study the condition. Previously, cases were often lumped into broader gastrointestinal or vomiting categories, obscuring the true prevalence and nature of CHS.
Beatriz Carlini, a research associate professor at the University of Washington School of Medicine, highlights the immediate benefits. “It helps us count and monitor these cases,” she explains, noting that a new code will provide crucial “hard evidence on cannabis-adverse events, which physicians tell us is a growing problem.” This enhanced surveillance will dramatically improve understanding of CHS, help pinpoint trends, and ultimately save lives, especially as cannabis legalization continues to spread and high-potency products become even more accessible.
Frequently Asked Questions
What exactly is Cannabis Hyperemesis Syndrome (CHS) and what are its key symptoms?
Cannabis Hyperemesis Syndrome (CHS) is a condition affecting chronic, long-term cannabis users, characterized by severe, recurrent episodes of nausea, intense vomiting, and abdominal pain. A hallmark symptom is “scromiting,” where individuals scream while vomiting due to extreme discomfort. Other symptoms include dehydration and weight loss. In severe instances, it can lead to dangerous complications like kidney failure, seizures, and heart rhythm abnormalities. Diagnosing CHS has been historically challenging due to its symptoms mimicking other common gastrointestinal issues.
Why are emergency room visits for CHS increasing so dramatically across the U.S.?
Emergency room visits for CHS have surged by approximately 650% since 2016, with numbers remaining high post-pandemic, particularly among young adults (18-35) and adolescents. Experts attribute this rise primarily to the widespread availability and use of high-potency cannabis products, which now often exceed 20% THC compared to 5% in the 1990s. Increased stress, isolation, and easier access to these potent products are also considered contributing factors. The formal WHO diagnostic code is expected to help better track and understand this alarming increase.
What is the most effective treatment for Cannabis Hyperemesis Syndrome, and are there any common misconceptions about it?
The only known effective treatment and “surefire cure” for CHS is the complete cessation of all cannabis use. Standard anti-nausea medications are typically ineffective. Some patients find temporary relief from hot showers or capsaicin cream applied to the abdomen, which are often used diagnostically. A common misconception is that CHS is not a real condition, making the new WHO diagnostic code crucial for its recognition. Many users also mistakenly attribute their intermittent episodes of illness to other causes, leading them to continue cannabis use and suffer recurring symptoms.
Conclusion
The formal recognition of Cannabis Hyperemesis Syndrome marks a pivotal moment in public health. With ER cases surging and high-potency cannabis products readily available, understanding this mysterious vomiting disorder is more crucial than ever. While the exact mechanisms are still being studied, evidence strongly links chronic, heavy use of high-THC cannabis to CHS. For those experiencing its debilitating symptoms, the message from health experts is clear: seeking accurate diagnosis and, critically, discontinuing cannabis use are the essential steps toward recovery. This new diagnostic code will undoubtedly empower medical professionals and researchers to better combat CHS, ultimately improving patient outcomes and public health awareness.