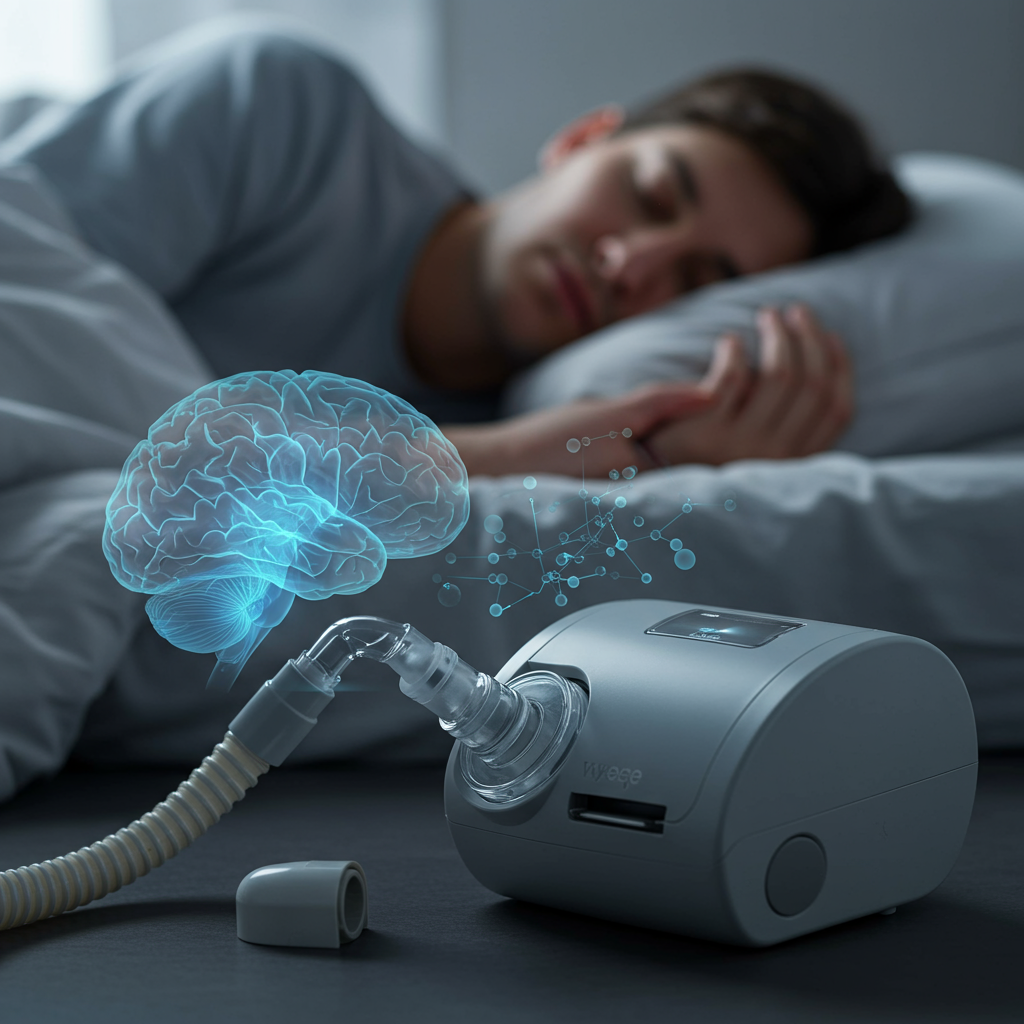
Are you one of the millions who dismiss loud snoring as just a harmless quirk? Perhaps you’ve been advised to use a CPAP machine for obstructive sleep apnea (OSA) but find it too inconvenient. It’s time to take a closer look, because new research reveals a compelling and urgent link between untreated sleep apnea and serious brain health risks, including an increased risk of dementia and Alzheimer’s disease.
This isn’t just about a good night’s sleep anymore. Emerging studies indicate that moderate to severe obstructive sleep apnea is significantly associated with a greater risk for new microbleeds in the brain. These tiny hemorrhages, often unseen, are now recognized as critical markers of brain aging and potential future cognitive decline. Ignoring your sleep apnea could have profound consequences for your long-term brain health.
The Unseen Threat: Understanding Brain Microbleeds
Cerebral microbleeds (CMBs) are small, chronic hemorrhages that occur in the brain’s tiny blood vessels. While they may not cause immediate symptoms, their presence is a significant concern. Dr. Jonathan Graff-Radford, a professor of neurology at Mayo Clinic College of Medicine, who was not involved in the latest research, notes that microbleeds are a common finding in the aging brain. “Anything that increases microbleeds is relevant to brain aging,” he explains.
Why are microbleeds so concerning? Their presence is linked to a slightly elevated risk of future strokes and a faster rate of cognitive decline. Essentially, these tiny bleeds are red flags, signaling underlying microvascular damage that can pave the way for more severe neurological issues later in life. This connection highlights why addressing factors that contribute to microbleeds, like untreated sleep apnea, is so crucial.
What Exactly is Obstructive Sleep Apnea?
Obstructive sleep apnea (OSA) is a common, yet often undiagnosed, sleep disorder. It occurs when the soft tissues in your throat – such as your tongue, tonsils, or palate – relax, become heavy, or are simply weak, causing a blockage in your airway during sleep. This blockage leads to repeated pauses in breathing, known as apneas, or shallow breathing, known as hypopneas. These episodes can last for seconds and happen many times an hour, severely disrupting your sleep quality and oxygen levels.
It’s important to distinguish OSA from central sleep apnea, where the brain occasionally fails to send proper signals to the muscles that control breathing. With OSA, the brain is trying to breathe, but the airway is physically blocked. This distinction is crucial for diagnosis and treatment.
Deeper Insights: OSA’s Independent Role in Brain Damage
While the initial study establishes a strong association, deeper research provides even more compelling evidence for why addressing OSA is so vital for brain health. A separate study published in Frontiers in Oncology explored the prevalence of cerebral microbleeds and their link to cognitive decline in patients with acromegaly, a condition marked by excess growth hormone. While acromegaly is a specific endocrine disorder, the study yielded a critical insight: obstructive sleep apnea was independently associated with an increased prevalence of CMBs, even after accounting for other factors like age, BMI, diabetes, and hypertension.
The findings were striking: acromegaly patients had significantly more CMBs (29.1% vs. 5.7% in healthy controls) and a very high rate of OSA (65.5%). Crucially, the study showed that the presence of OSA increased the odds of having CMBs by a staggering 13.34 times in this population. This suggests a powerful, direct pathway: the persistent disruptions from OSA, likely through mechanisms like chronic intermittent hypoxia (low oxygen) and fluctuations in blood pressure, directly contribute to microvascular damage, leading to more numerous and often more severe microbleeds. What’s more, CMBs in acromegaly patients were found at a younger age and predominantly in lobar regions of the brain, suggesting an accelerated process of cerebral small vessel injury. This robust evidence from a specific patient group strongly reinforces the concern for the general population: OSA isn’t just a byproduct; it’s an active contributor to brain microvascular damage.
The “Double Whammy” Effect on Your Brain
Dr. Rudy Tanzi, a professor of neurology at Harvard Medical School and director of the Genetics and Aging Research Unit at Massachusetts General Hospital, who also reviewed the initial study, describes untreated obstructive sleep apnea as a “double whammy” for brain health. First, impaired breathing during the night leads to chronically poor sleep quality. This alone has been independently linked to accelerated brain aging and an increased risk of neurodegenerative diseases. Sleep is when your brain clears out waste products, consolidates memories, and repairs itself. Without quality sleep, these vital processes are compromised.
Second, the microbleeds that can result from OSA further compound this risk, increasing the likelihood of dementia and Alzheimer’s disease down the line. It’s not just about feeling tired; it’s about the tangible damage occurring within your brain that can have irreversible consequences.
Spotting the Signs: When to Talk to Your Doctor
The message from experts is clear: “Don’t ignore it. Do something about it.” But how do you know if you might have obstructive sleep apnea? While a formal diagnosis requires a sleep study, several common signs and symptoms should prompt a conversation with your doctor.
Keep an eye out for these key indicators:
Loud, Frequent Snoring: This is often the most noticeable sign.
Witnessed Breathing Pauses: If your partner observes you stopping breathing, gasping, or choking during sleep, it’s a strong red flag.
Daytime Sleepiness: Feeling excessively tired, even after a full night’s sleep.
Difficulty Concentrating: Trouble focusing, memory issues, or a general “brain fog.”
Irritability and Mood Changes: Lack of quality sleep can significantly impact your emotional regulation.
Increased Hunger: Sleep deprivation can disrupt hormones that regulate appetite.
Night Sweats: Research shows about 30% of people with OSA report night sweats.
Frequent Night Wakings: Waking up two or more times during the night, often to use the restroom.
Teeth Grinding (Bruxism): Can be a symptom of disrupted sleep and airway issues.
Morning Headaches: Waking up with a headache can be due to reduced oxygen during sleep.
If you recognize several of these symptoms, it’s time to get assessed for obstructive sleep apnea. Early diagnosis and treatment are your best defense against potential long-term brain damage.
Taking Action: Effective Treatment Options
Fortunately, obstructive sleep apnea is a treatable condition. A range of effective interventions can help keep your airways open, restore healthy breathing patterns, and protect your brain.
Common treatment approaches include:
Continuous Positive Airway Pressure (CPAP) Machine: This is the most common and often most effective treatment. A CPAP machine delivers a gentle stream of air through a mask worn during sleep, keeping your airway open. While some find it cumbersome initially, consistent use can dramatically improve sleep quality and overall health.
Oral Devices: Custom-made mouthpieces, similar to athletic mouthguards, can help reposition your jaw or tongue to keep the airway open. These are often suitable for mild to moderate OSA.
Lifestyle Changes: Losing weight (if overweight), avoiding alcohol and sedatives before bed, quitting smoking, and sleeping on your side can all help reduce OSA severity.
Positional Therapy: Devices that encourage sleeping on your side can prevent back-sleeping, which often worsens OSA.
Surgery: In some cases, surgical procedures may be recommended to remove excess tissue, reposition the jaw, or address structural issues contributing to the airway blockage.
Emerging Therapies: Newer options, such as hypoglossal nerve stimulation devices, are also becoming available for specific patients who can’t tolerate CPAP.
Working with your doctor or a sleep specialist is crucial to determine the best treatment plan for your individual needs. Remember, the goal is not just to stop snoring but to ensure continuous, healthy breathing throughout the night.
Frequently Asked Questions
What exactly are brain microbleeds, and how do they relate to sleep apnea?
Brain microbleeds (CMBs) are tiny hemorrhages in the small blood vessels of the brain, often undetectable without specialized MRI. They are radiographic markers of microvascular injury, indicating damage to the brain’s delicate blood supply. Studies show that obstructive sleep apnea (OSA) is strongly associated with an increased risk of developing new CMBs. Experts like Dr. Jonathan Graff-Radford note that CMBs are linked to a higher risk of future strokes and faster cognitive decline, making their increase due to OSA a significant concern for long-term brain health and dementia risk.
Where can I get tested or find treatment options for obstructive sleep apnea?
If you suspect you have obstructive sleep apnea based on symptoms like loud snoring, daytime fatigue, or observed breathing pauses, your first step should be to consult your primary care physician. They can refer you to a sleep specialist or a sleep clinic. Diagnosis typically involves a sleep study (polysomnography), which can be done in a lab or sometimes at home. Treatment options, including CPAP machines, oral devices, or surgery, are usually prescribed and managed by sleep specialists, often in collaboration with ear, nose, and throat (ENT) doctors or oral surgeons.
Should I be worried about dementia if I have sleep apnea, and what’s the best next step?
While the studies establish an association and not definitive causation between OSA, microbleeds, and dementia, the link is significant enough to warrant serious concern. Dr. Rudy Tanzi highlights OSA as a “double whammy,” where poor sleep quality and potential microbleeds collectively elevate the risk for dementia and Alzheimer’s disease. The best next step is to act promptly: if you experience symptoms of sleep apnea, consult your doctor for a diagnosis. Early and consistent treatment can mitigate these risks, improve your overall health, and protect your brain from potential long-term damage, emphasizing the importance of taking sleep apnea seriously now.
Protect Your Brain: Act Now on Sleep Apnea
The latest research paints a clear picture: what happens during your sleep has a direct and profound impact on your brain’s long-term health. Obstructive sleep apnea is not merely an inconvenience; it’s a serious medical condition with the potential to contribute to brain microbleeds, accelerate cognitive decline, and increase your risk of dementia and Alzheimer’s disease.
Don’t let perceived inconvenience or a lack of urgency keep you from addressing this critical health issue. The strong, independent association between OSA and cerebral microbleeds, particularly highlighted in comprehensive research, urges immediate attention. By recognizing the signs, seeking a diagnosis, and committing to an effective treatment plan, you can significantly reduce these risks, improve your quality of life, and safeguard your most valuable asset: your brain. Take action today for a healthier tomorrow.