For decades, the mystery of phantom limbs – the vivid sensation of a missing body part – has baffled scientists and tormented amputees. A groundbreaking new study, published in Nature Neuroscience, now fundamentally reshapes our understanding. It reveals that the brain’s detailed body map remains surprisingly stable after amputation, directly challenging long-held beliefs about brain reorganization and offering a new path forward for treating phantom limb pain and developing advanced prosthetics. This research promises to revolutionize patient care and neuro-technologies.
The Enduring Enigma of Phantom Limbs
Imagine losing a limb, yet still feeling its presence, sometimes agonizingly so. This is the reality for most amputees experiencing phantom limbs. The human brain houses an intricate “body map,” with distinct zones dedicated to every body part. Historically, scientists believed that when a limb was lost, this brain map dramatically rewired itself. The area previously dedicated to the missing limb was thought to be “taken over” by neighboring body parts, a concept central to adult brain plasticity. This idea suggested the brain aggressively reorganizes in response to injury.
This long-standing theory also served as the primary explanation for phantom limb pain. The logic was that a “broken” or reorganized brain map somehow generated the burning, stabbing, or itching sensations. Consequently, many therapies were designed to “fix” these supposed brain map errors. Treatments like mirror box therapy, virtual reality training, and sensory-discrimination exercises aimed to correct the assumed neural disarray. However, their consistent failure to outperform placebo treatments in clinical trials hinted at a deeper misunderstanding.
Challenging Decades of Dogma: The New Discovery
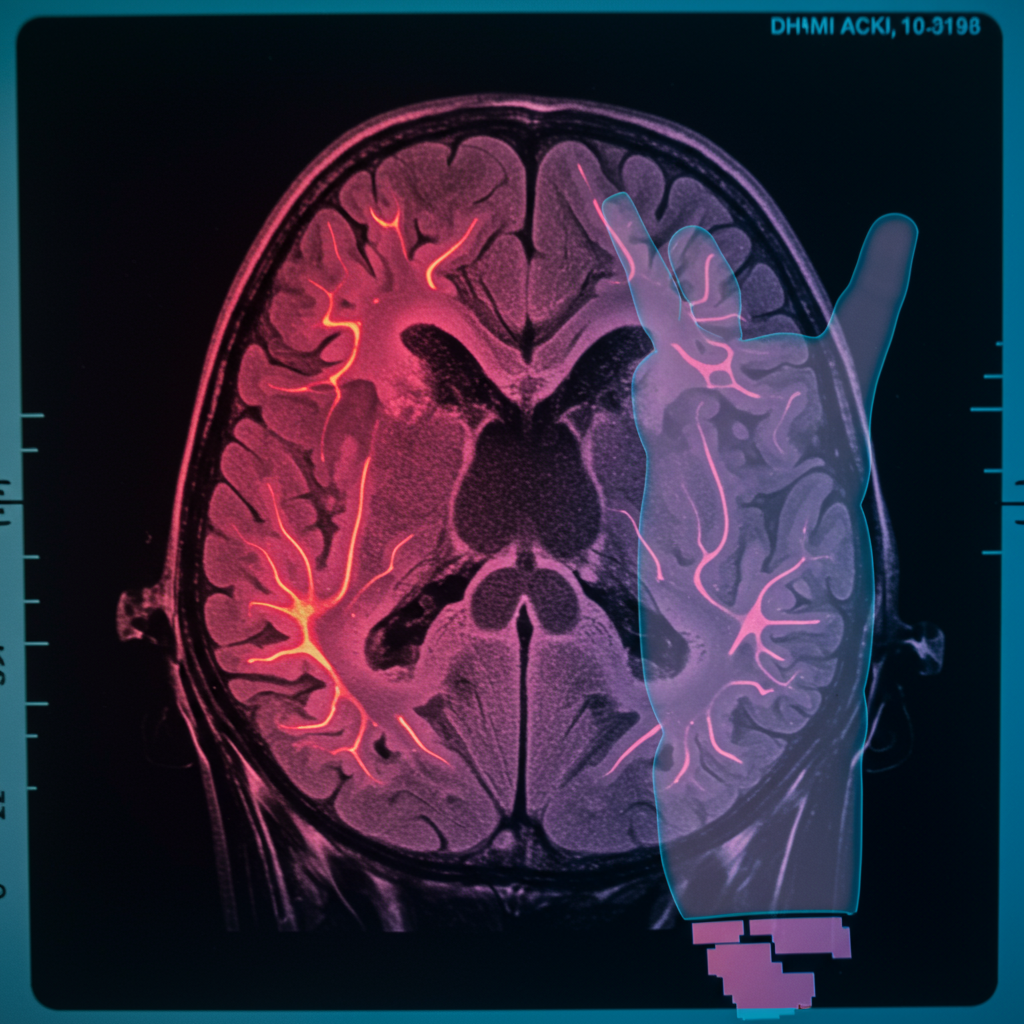
The new research delivers a powerful counter-narrative. It shows precisely the opposite: the brain’s body map for an amputated limb stays remarkably intact. Researchers followed three adult patients undergoing life-saving arm amputations. They conducted functional magnetic resonance imaging (fMRI) brain scans both before and repeatedly after surgery, spanning up to five years. This unique pre- and post-amputation comparison in the same individuals provided unprecedented insights.
Unpacking the Revolutionary Approach
During the fMRI scans, patients were asked to perform specific movements. Before surgery, they tapped individual fingers, curled toes, or pursed lips. This allowed researchers to meticulously map their brain activity. After the amputation, a crucial step involved asking patients to “move” their missing (phantom) fingers. Phantom movements are not mere imagination; many amputees genuinely feel these vivid sensations. This innovative technique provided a direct comparison of the brain’s hand map before and after the physical loss of the limb.
The Brain’s Unexpected Stability
The results were consistent across all three patients. The neural map of the hand in their brains remained strikingly unchanged. There was no evidence of it being overwritten or taken over by other body parts, such as the face. This profound neural stability offers a compelling explanation for why so many amputees continue to experience such vivid sensations of their missing limbs. The limb, in essence, continues to “live on” within the brain’s representation. This finding directly refutes the long-held reorganization theory, prompting a critical reevaluation of our understanding of brain plasticity in this context.
Rethinking Phantom Limb Pain: The True Culprit
The implications of this discovery are vast. If the brain’s body map isn’t broken, then attempting to “fix” it through therapies based on the reorganization theory is a dead end. This new understanding helps clarify why many existing treatments for phantom limb pain have limited success. It shifts the focus away from the brain’s central processing and towards a more peripheral origin for the discomfort.
Why Current Therapies Fall Short
Therapies like mirror box exercises, which encourage visual feedback to “trick” the brain into believing the missing limb is present and moving, were predicated on the idea of correcting a reorganized map. Similarly, virtual reality training and sensory-discrimination exercises aimed to restore a supposedly disturbed neural representation. The new study suggests these approaches were fundamentally misguided. If the brain’s map is stable, these interventions cannot target the root cause of pain. This doesn’t mean patients haven’t found relief through them, but rather that the mechanism of action might be different, or the relief might be akin to a placebo effect, as clinical trials often show.
Pinpointing the Peripheral Problem
Instead of a rewired brain, the study points to the peripheral nervous system as the likely “real culprit” for painful phantom sensations. During amputation, nerves are severed. These cut nerves can sometimes form tangled clusters, known as neuromas. These neuromas can then misfire signals back to the brain, creating aberrant, painful sensations that are misinterpreted as originating from the missing limb. This peripheral nerve hypothesis is gaining traction. New amputation surgical techniques are now being developed specifically to preserve nerve signaling and maintain stable connections to the brain, aiming to prevent these misfiring signals from ever forming. These techniques could significantly reduce the incidence and severity of phantom limb pain.
A Future of Hope: Next-Gen Prosthetics and BCIs
The discovery of the brain’s stable body map holds immense promise for future technological advancements. It provides a critical neural resource for developing more intuitive and effective prosthetic limbs and advanced brain-computer interfaces (BCIs).
Leveraging the Brain’s Intact Map
Invasive Next-Generation BCIs: These technologies can directly tap into the preserved neural map of the amputated body part. By doing so, they can decode the specific movements an amputee intends to make with their missing limb. This decoded intention can then be translated into commands for a prosthetic limb, allowing for natural and intuitive control.
Sensory Feedback: Beyond control, the preserved map can also receive electrical stimulation. This stimulation, delivered directly to the brain’s representation, could enable amputees to feel their prosthetic limb. Imagine not just moving a prosthetic hand, but feeling its grip, temperature, or texture – restoring a sense of embodiment.
Paving the Way for Breakthroughs
These cutting-edge technologies are currently in various stages of development. They offer the potential to fundamentally transform the lives of amputees by restoring not just function, but also natural sensation and intuitive control over their artificial limbs. The brain’s resilient model of the body, maintaining these representations even after sensory input is lost, proves to be an invaluable asset. For amputees, the missing limb lives on within their brain, presenting both a challenge (in terms of discomfort) and an extraordinary opportunity for future technologies. This shift in scientific understanding promises a brighter, more integrated future for those living with limb loss.
Frequently Asked Questions
How does the latest research change our understanding of phantom limb pain?
The recent study fundamentally shifts our understanding by showing the brain’s body map for an amputated limb remains remarkably stable, rather than reorganizing as previously believed. This neural stability explains why amputees feel vivid sensations. It suggests phantom limb pain isn’t due to a “broken” brain map, but more likely from misfiring signals in severed peripheral nerves at the amputation site. This challenges decades of scientific dogma and redirects research towards nerve-focused interventions.
Which existing phantom limb therapies are now considered less effective, and why?
Therapies like mirror box therapy, virtual reality training, and sensory-discrimination exercises, which were designed to “fix” a supposedly reorganized brain map, are now viewed as less effective in addressing the root cause of phantom limb pain. The new research indicates that since the brain’s body map remains intact, these methods are not targeting the actual problem. Their limited success in clinical trials, often no better than placebo, aligns with this revised understanding.
What new treatment approaches or technologies are being explored for amputees based on this discovery?
Based on the discovery of the brain’s stable body map, new approaches focus on the peripheral nerves and advanced prosthetics. Surgical techniques are developing to preserve nerve signaling and prevent misfiring, potentially reducing pain. For prosthetic limbs, next-generation brain-computer interfaces (BCIs) are being designed to tap into the preserved brain map. This allows for intuitive control of prosthetics and even direct electrical stimulation to the brain to restore natural sensations, offering hope for more integrated and functional artificial limbs.
Conclusion
The groundbreaking research into phantom limbs marks a significant turning point in neuroscience. By demonstrating the enduring stability of the brain’s body map, even years after amputation, scientists are overturning long-held theories. This paradigm shift not only explains the persistence of vivid phantom sensations but also redefines the origins of phantom limb pain, pointing towards peripheral nerve issues rather than central brain reorganization. The implications are profound, paving the way for targeted surgical advancements and the development of revolutionary brain-computer interfaces and prosthetic limbs. This deeper understanding of the brain’s resilience offers immense hope, transforming the missing limb from a source of suffering into a vital neural resource for future innovation.