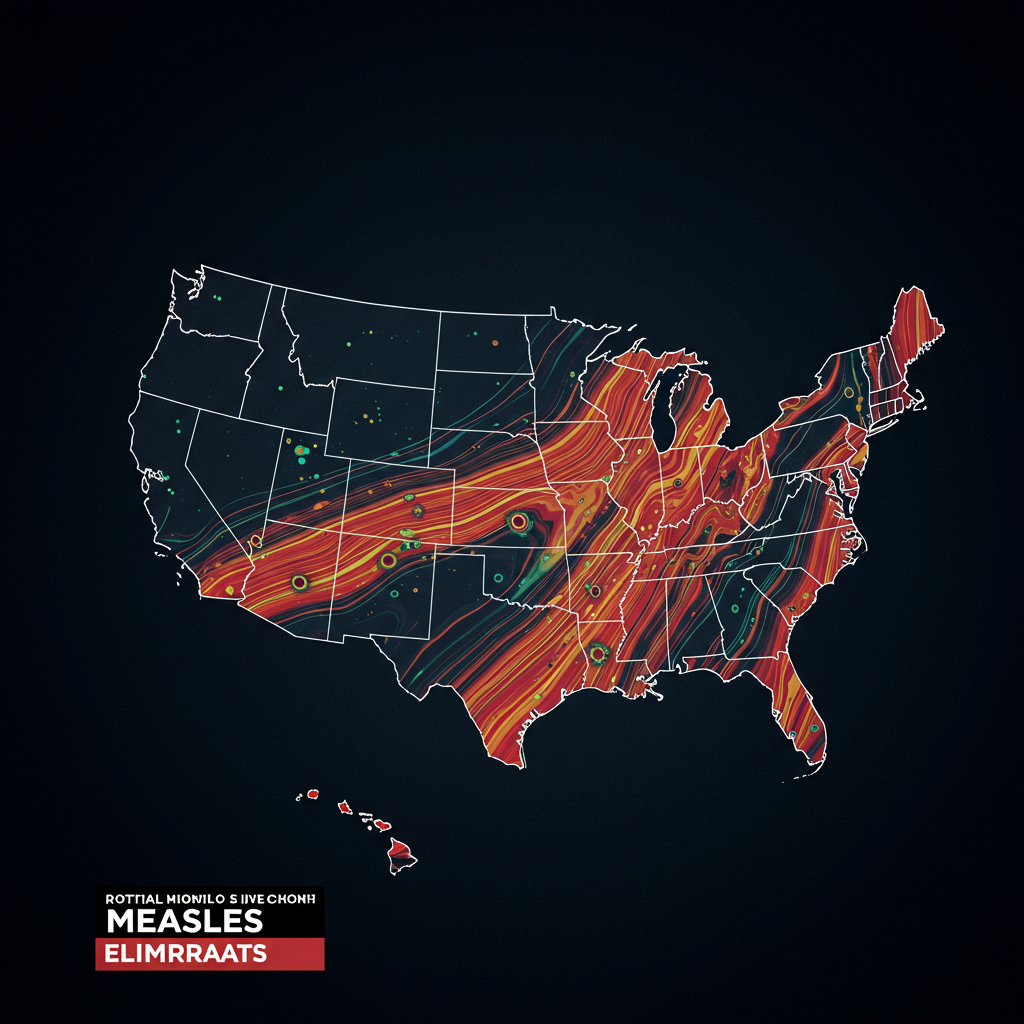
The United States is rapidly approaching a critical public health milestone, one that signals a concerning reversal of decades of progress: the potential loss of its official measles elimination status. Weekly updates from the Centers for Disease Control (CDC) reveal a steady climb in cases, pushing the nation closer to a grim, seemingly unavoidable reality.
Driven significantly by a prolonged, multi-state outbreak centered in West Texas, this year’s measles count has already surpassed 1,200 cases, tragically including three deaths. This trajectory indicates the U.S. is on track to exceed the case total from 2019 – a year when measles outbreaks dominated headlines, strained healthcare systems, and prompted emergency responses, offering an unsettling preview of the challenges the nation would soon face with COVID-19.
Why the U.S. Is More Vulnerable Now
Experts warn that the U.S. public health landscape is in a more precarious state today than it was during the 2019 outbreaks. A significant factor is the increasingly polarized confidence in public health measures, particularly vaccinations, often split along political lines.
The national measles-mumps-rubella (MMR) vaccination rate among kindergarteners has dropped below 93% and continues to fall. While 95% coverage is generally considered the threshold needed to prevent outbreaks, this national figure doesn’t tell the whole story. Critically low vaccination rates at local levels – in specific counties, cities, or even neighborhoods – are sufficient to allow continuous spread of the highly contagious virus for months or even years. For instance, while the Texas statewide MMR rate is 94%, Gaines County, the epicenter of the major outbreak, reports a local rate closer to 80%.
A Hard-Won Victory Now at Risk
The ability to prevent measles has existed for over 60 years, with the first vaccines licensed in 1963. However, achieving elimination – meaning interrupting ongoing transmission throughout the country, allowing only imported cases that didn’t spark widespread outbreaks – was a much longer and more challenging journey. Built on hard-won knowledge from large outbreaks in the 1970s, ’80s, and ’90s, elimination was finally achieved in 2000.
This success was the result of key strategies developed through painful lessons, including:
Recognizing the need for two doses of the MMR vaccine.
Implementing crucial school vaccination mandates.
Leveraging federal funding like the Vaccines for Children program.
Strengthening local public health departments to improve access to vaccines.
These interventions, forged in the aftermath of suffering and preventable childhood deaths, represent a delicate system built over decades.
Threats to Maintaining Elimination Status
Maintaining measles elimination requires constant vigilance: encouraging parents to vaccinate, robust disease surveillance, and well-resourced public health agencies capable of quickly identifying and controlling outbreaks. Alarmingly, this entire system is currently under significant threat.
Modeling studies suggest that even if current vaccination rates hold steady, the U.S. is likely to lose its hard-won elimination status. This outcome becomes a near certainty if rates continue their decline and could happen within the next year if current outbreaks persist.
Threats stem not only from a well-funded and increasingly emboldened anti-vaccine movement but also from actions observed within federal public health agencies themselves. Recent events, such as the removal and replacement of expert advisory committee members with individuals potentially tied to anti-vaccine views, highlight the perilous state of vaccination efforts in the U.S. today.
More Than Just Measles
Surpassing the 2019 case count and potentially losing elimination status are deeply symbolic moments. They signify a stark reversal, a return to a time when measles hospitalizations and childhood deaths were tragically common, shattering families with this preventable disease every single year.
These symbols also carry meaning beyond measles itself. They signal the potential re-emergence of other vaccine-preventable diseases that America had largely forgotten. Measles is often the first to reappear due to its extreme contagiousness, but others are already following suit. Pertussis (whooping cough) is surging, causing preventable infant deaths in states with reduced vaccination promotion. Cases of severe, vaccine-preventable Hib meningitis have also been reported in unvaccinated children in recent years.
The U.S. stands on the precipice of returning to a past marked by unspeakable, yet preventable, tragedy for children and families. Averting this fate may depend critically on the collective voice and actions of parents and grandparents, united across political and geographic divides.