Imagine developing a sudden, severe allergy to steak, burgers, or even bacon. For a growing number of Americans, this isn’t a hypothetical scenario but a frightening reality brought on by a tick bite. Experts are sounding the alarm over the significant rise and spread of <a href="https://news.quantosei.com/2025/06/29/how-to-protect-yourself-from-ticks-year-round/” title=”Essential Ways to Protect From Ticks Year-Round”>alpha-gal Syndrome (AGS), a mysterious illness transmitted by ticks that causes a delayed, potentially life-threatening allergic reaction to red meat and other mammalian products.
What is Alpha-Gal Syndrome (AGS)?
Alpha-Gal Syndrome, or AGS, is an allergic condition triggered by the bite of certain ticks, most commonly the Lone Star tick in the United States. These ticks carry a sugar molecule called alpha-gal. When an alpha-gal carrying tick bites a human, it injects this sugar into the bloodstream. The human immune system recognizes alpha-gal as foreign and develops antibodies to fight it off.
The challenging part is that alpha-gal molecules are also naturally present in the meat of most mammals, such as beef, pork, lamb, and venison. They are also found in mammalian-derived products like dairy milk, gelatin, and certain medications. If a person with alpha-gal antibodies consumes these foods or products, their body launches an immune attack against the alpha-gal, leading to an allergic reaction.
The Expanding Threat: Why Cases Are On the Rise
The number of documented Alpha-Gal Syndrome cases has surged dramatically. According to the CDC, over 110,000 cases have been recorded since 2010. However, health officials estimate the true number could be significantly higher, potentially reaching 450,000, due to underreporting and frequent misdiagnoses. This suggests a vast, mostly hidden public health challenge.
Experts confirm these numbers are not just high, but rapidly increasing. Brandon Hollingsworth, a tick expert at the University of South Carolina, notes that what seemed rare a decade ago has become increasingly common and expects this rapid growth to continue. This rise is closely linked to environmental factors, particularly climate change. Warmer temperatures and milder winters allow ticks to survive longer and expand their geographical reach.
Historically, AGS cases were concentrated in specific regions like the southern, midwestern, and mid-Atlantic United States. However, recent studies on tick and human samples indicate millions more Americans could be at risk. The ticks responsible for AGS are spreading into new territories. Laura Harrington, a disease specialist at Cornell, points out the adaptive nature of these ticks combined with rising temperatures suggests few natural limits to their future spread. Alarmingly, the condition is also being traced to new tick species previously not associated with transmitting alpha-gal. Hollingsworth warns of an “explosive increase” in these ticks, predicting that the range of alpha-gal risk could encompass the entire eastern half of the US, potentially impacting millions with this peculiar allergy.
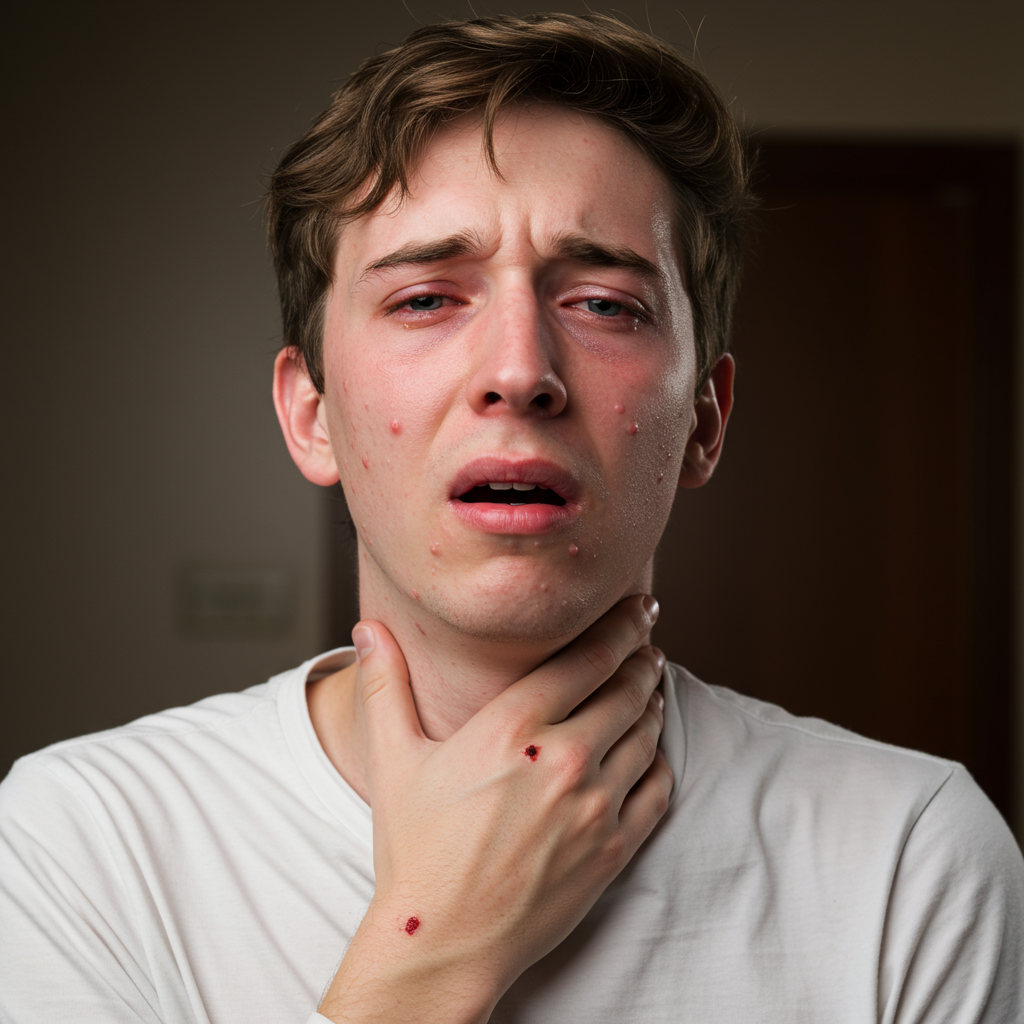
Understanding the Delayed and Variable symptoms
One of the most confusing aspects of Alpha-Gal Syndrome is the timing of symptoms. Unlike immediate allergies, AGS reactions typically appear between two and six hours after consuming mammalian meat or products containing alpha-gal. This significant delay makes it difficult for affected individuals and even doctors to immediately connect the reaction to a recent meal, let alone a tick bite that might have occurred weeks or months earlier.
The symptoms themselves can vary widely in severity and type. Common signs include:
Hives or an itchy rash
Nausea and vomiting
Heartburn or indigestion
Diarrhea and stomach pain
Shortness of breath or difficulty breathing
Dizziness or lightheadedness
Swelling of the lips, tongue, throat, or eyelids
In more severe instances, the reaction can escalate to anaphylaxis, a life-threatening condition requiring immediate medical attention. Some highly sensitive individuals have even reported symptoms after merely inhaling fumes from cooking mammalian meat.
A notable case study highlighted the potential danger. A 61-year-old woman experienced two major allergic episodes after eating beef and pork tacos. Her first reaction, which occurred nearly a month after a tick bite, was relatively mild, involving hives and swelling. However, a month later, a second reaction was far more severe. Her tongue swelled to the point she couldn’t speak, her blood pressure dropped dangerously low, and her heart rate soared. She required hospitalization and aggressive treatment with epinephrine and steroids to recover. This case underscores how AGS reactions can worsen over time and the critical challenge posed by the delayed link between the tick bite and the allergic symptoms.
The Broader Landscape of Tick-Borne Threats
Alpha-Gal Syndrome is not the only concern carried by ticks. Ticks are significant vectors for a variety of diseases, second only to mosquitoes globally. In the U.S. alone, tick-borne illnesses account for over 80% of reported vector-borne disease cases. While Lyme disease is the most well-known, with estimated actual cases potentially reaching half a million annually despite lower reported numbers, ticks transmit at least 17 different known human pathogens. In the last two decades, six new tick-borne illnesses have been identified, highlighting the evolving nature of this threat, partly due to increased health professional awareness.
The overall increase in tick populations and the diseases they carry is a complex issue driven by factors like climate change expanding tick habitats, greater overlap between human communities and wildlife areas (like deer and rodents that host ticks), and the ticks’ own adaptive abilities.
Protecting Yourself: Essential Prevention Steps
Preventing tick bites remains the most effective way to avoid AGS and other tick-borne illnesses. Experts recommend incorporating vigilance into your outdoor routine, especially in known tick habitats like wooded, bushy, or tall grassy areas.
Key prevention strategies include:
Wear Protective Clothing: When venturing outdoors, wear long-sleeved shirts and long pants. Tuck your pants into your socks to create a barrier.
Use Repellents: Apply EPA-registered insect repellents containing DEET to exposed skin. You can also treat clothing and gear with products containing permethrin (follow instructions carefully, do not apply directly to skin).
Avoid Risky Areas: Try to avoid walking through thick brush or tall grass where ticks are likely to hide. Stay on marked trails.
Check Clothing: After spending time outdoors, put your clothes in a dryer on high heat for at least 10 minutes to kill any ticks that may be attached.
Perform a Thorough Body Check: Conduct a full-body check upon returning indoors. Pay close attention to areas like the scalp, ears, inside elbows, backs of knees, armpits, and groin. Ticks can be very small, especially in their nymph stage.
Check Pets: Dogs and other pets can carry ticks into your home. Check them regularly, especially after they’ve been in tick-prone areas.
Remove Ticks Properly: If you find a tick attached, remove it as soon as possible. Use fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible. Pull upward with steady, even pressure. Avoid twisting or jerking. Do not use folklore remedies like matches, nail polish, or petroleum jelly, as these can irritate the tick and cause it to release more pathogens.
Clean the Bite Area: After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.
Monitor for Symptoms: Keep an eye on the bite area for any rash and monitor your health for several weeks. If you experience flu-like symptoms, unusual rashes, or allergy-like symptoms (especially after eating mammalian meat), consult a healthcare provider. Be sure to mention your tick exposure.
The Public Health Response Challenge
Despite the growing threat of Alpha-Gal Syndrome and other vector-borne diseases, the U.S. public health system faces significant challenges in surveillance, prevention, and response. Underreporting and misdiagnosis mask the true scale of the problem. Funding for vector-borne disease control and research has been inconsistent and often reactive, increasing only after major outbreaks rather than proactively building capacity. State and local health departments often lack the necessary resources for robust surveillance and control programs. Healthcare providers in areas newly affected by expanding tick ranges may not be familiar with diagnosing or treating conditions like AGS.
While efforts are underway, such as the national strategy mandated by the Kay Hagan Tick Act, implementing these strategies effectively requires sustained funding and coordinated action across federal, state, and local levels. Increased public and professional awareness about AGS and tick prevention is also critical to curb its spread and impact.
Frequently Asked Questions
How does a tick bite cause a meat allergy?
A tick bite, most commonly from the Lone Star tick in the U.S., can transmit a sugar molecule called alpha-gal into a person’s bloodstream. The human immune system doesn’t typically have this sugar and sees it as a foreign invader. This triggers an immune response, creating specific antibodies against alpha-gal. Since this same alpha-gal sugar is found in the meat and products of mammals (like beef, pork, venison, milk, gelatin), when a person with these antibodies later consumes these items, their body reacts allergically to the alpha-gal present.
What should I do if I find a tick or think I might have AGS?
If you find a tick attached, remove it promptly and correctly using fine-tipped tweezers, pulling straight up close to the skin. Clean the bite area. Monitor the bite site for a rash and watch for any unusual symptoms in the following weeks, especially if you consume mammalian meat. If you develop symptoms consistent with AGS (hives, GI issues, breathing problems) or flu-like symptoms after a potential tick exposure, consult a doctor. Inform them about the tick bite, even if it happened weeks or months earlier, as the link isn’t always obvious.
How serious is Alpha-Gal Syndrome and what are the risks?
Alpha-Gal Syndrome can range from mild to severe. Symptoms often include hives, digestive upset, or swelling. However, reactions can escalate to life-threatening anaphylaxis, involving severe breathing difficulties and a dangerous drop in blood pressure. The delayed onset (hours after eating meat) makes it particularly risky because treatment can be delayed if the cause isn’t recognized quickly. While confirmed deaths directly attributed solely to AGS are not widely reported by health officials, the potential for severe allergic reactions poses a significant health risk for affected individuals.
Conclusion
Alpha-Gal Syndrome represents a concerning and rapidly growing public health challenge across the United States. Driven by expanding tick populations linked to climate change and other environmental factors, this tick-borne illness can trigger debilitating and potentially severe allergic reactions to red meat and mammalian products. The delayed onset of symptoms complicates diagnosis, making awareness and prevention crucial. By understanding the risks, taking proactive steps to prevent tick bites, and recognizing the signs and symptoms, individuals can better protect themselves and seek appropriate medical care if needed. As ticks continue to spread, vigilance and increased surveillance will be key in navigating this evolving threat.