The United States is currently grappling with a severe public health challenge: a dramatic resurgence of measles. In 2025, the nation recorded its highest number of measles cases in over three decades, threatening its hard-won status of disease elimination. This escalating crisis is fueled by declining vaccination rates and increasing vaccine hesitancy, creating a “perfect storm” for a highly contagious and potentially deadly illness. Understanding the current landscape, the risks involved, and the proven preventative measures is critical for safeguarding individual and community health across the United States.
The Alarming Surge: 2025 Marks a Decades-High Outbreak
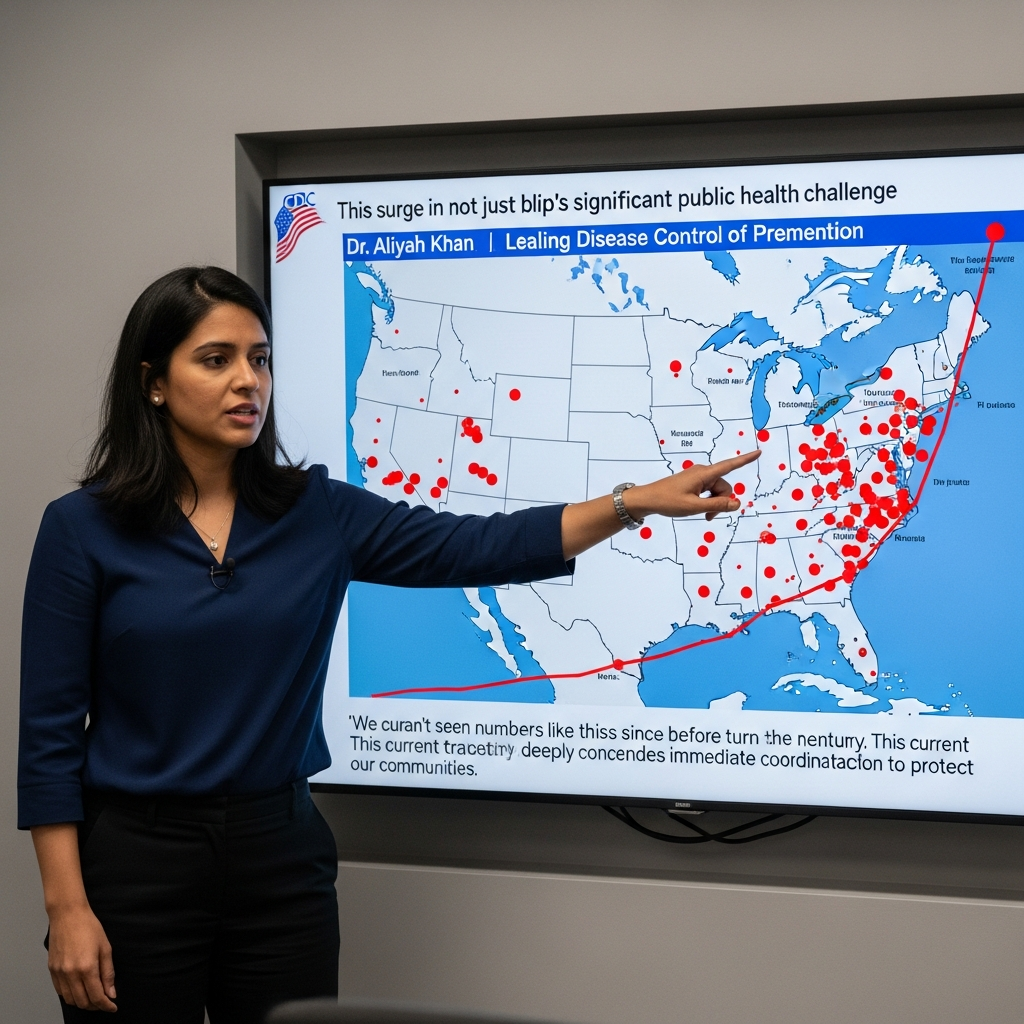
Official data from the Centers for Disease Control and Prevention (CDC) paints a stark picture of the US measles outbreak. By early July 2025, confirmed cases soared to 1,288, climbing further to 1,309 by mid-July. This made 2025 the year with the highest measles caseload since 1992. The numbers continued their upward trajectory, reaching 1,356 across 42 jurisdictions by August 12, and an alarming 1,912 confirmed cases by December 9, 2025 – the highest since 2000, the year measles was declared eliminated in the U.S.
The outbreak has been widespread, impacting at least 39 states. Texas has been particularly hard hit, reporting 753 cases, while South Carolina accounted for a significant 129 cases. Tragically, this resurgence also led to three measles-related deaths in 2025, underscoring the disease’s severe potential.
A Critical Factor: Unvaccinated Individuals at Risk
A consistent and critical finding across these outbreaks is the vaccination status of those affected. A staggering 92% of the confirmed measles patients in 2025 were either unvaccinated against the disease or had an unknown vaccination history. This data clearly highlights the vulnerability of non-immunized populations to this highly contagious virus.
The age distribution of cases in 2025 also presented a concern, with approximately 25% of cases occurring in children under five years old and a notable 33% in adults over 20. Experts attribute this to “long-standing undervaccination in some communities,” indicating pockets of susceptibility that allow the virus to gain a foothold and spread.
Why the Resurgence? Unpacking the Core Causes
The dramatic spike in measles cases US is not a random event; it’s the culmination of several interconnected factors that have eroded public health defenses built over decades.
Declining Vaccination Rates and Herd Immunity Breaches
One of the most significant contributing factors is the decline in childhood vaccination rates. For the 2023–24 school year, kindergarten vaccination rates for measles, mumps, and rubella (MMR) fell to 92.7%. This figure is critically below the 95% herd immunity threshold, which public health experts consider necessary to prevent widespread outbreaks. Herd immunity protects not only vaccinated individuals but also those who cannot be vaccinated due to age or underlying health conditions. When vaccination rates drop below this threshold, the entire community becomes more susceptible.
The Shadow of Vaccine Hesitancy
A growing wave of vaccine hesitancy, intensified during and after the COVID-19 pandemic, has played a substantial role. Misinformation and skepticism have led more parents to delay or refuse recommended childhood immunizations. While the Centers for Disease Control and Prevention (CDC) strongly recommends the MMR vaccine as the best protection, an Health and Human Services spokesperson noted that “The decision to vaccinate is a personal one,” reflecting the challenge of balancing public health recommendations with individual autonomy.
Global Interconnections: Importation Risks
The US measles outbreak cannot be viewed in isolation. A concurrent increase in measles cases internationally, with Europe experiencing its highest numbers in over 25 years and outbreaks spreading in Mexico and Canada, significantly raises the risk of importation. Unvaccinated individuals in the U.S. are highly vulnerable to measles imported via international travel, swiftly turning a global problem into a domestic crisis.
Measles: Beyond a Mild Childhood Rash
Often mistakenly perceived as a minor ailment, measles is far from benign. It is a serious, highly contagious disease with potentially severe complications.
Recognizable Symptoms and Dangerous Complications
Measles symptoms typically appear 10 to 14 days after exposure. They begin with a high fever, cough, runny nose, and red, watery eyes. A distinctive red, spotty rash then emerges, usually starting on the head and behind the ears, before spreading downwards across the body.
The virus can lead to severe health issues, including:
Pneumonia: A common and serious complication, especially in young children.
Ear Infections: Can lead to permanent hearing loss.
Diarrhea and Dehydration: Particularly dangerous for infants.
Encephalitis (Brain Swelling): Occurs in about 1 in 1,000 cases and can result in permanent disabilities such as blindness, deafness, or intellectual impairments.
- Death: Historically, 500 children died annually from measles in the U.S. before widespread vaccination. Currently, approximately 1 to 2 out of every 1,000 cases result in death. Globally, the World Health Organization reported 107,500 measles deaths in 2023, predominantly among unvaccinated or undervaccinated children under five.
- First Dose: Between 12 and 15 months of age, providing 95-97% protection.
- Second Dose: Between 4 and 6 years of age, boosting protection to about 99%.
- www.britannica.com
- conexiant.com
- conexiant.com
- health.ucdavis.edu
- www.britannica.com
Specific Risks for Vulnerable Populations
For pregnant individuals, measles carries significant risks, including an increased likelihood of intrauterine fetal death, spontaneous abortion, and maternal death. This underscores the importance of vaccination not only for children but also for adults, particularly those in childbearing years.
The Ultimate Defense: The MMR Vaccine
The most effective tool against measles remains the Measles, Mumps, and Rubella (MMR) vaccine. It uses live, weakened forms of the viruses to stimulate a protective immune response.
Recommended Schedule and Efficacy
The CDC recommends two doses of the MMR vaccine:
Children should receive both doses before entering school. Full vaccination is especially crucial for individuals planning international travel due to the global increase in cases. Most adults are considered immune either from having had measles as children or from vaccination. Those unsure of their immunity status should consult their healthcare providers, as there is no harm in receiving the vaccine even if already immune.
Debunking the Autism Myth
Concerns about a link between the MMR vaccine and autism arose from a now-discredited publication in 1998. Since then, numerous robust scientific studies involving millions of children across various countries have consistently and conclusively found no causal link between the MMR vaccine and autism. Public health authorities worldwide reaffirm the vaccine’s safety.
Treatment and Prevention Strategies
There is no specific antiviral treatment for measles. Care focuses on supportive measures, such as providing IV fluids for dehydration or supplemental oxygen for respiratory difficulties. Infected individuals should rest, drink plenty of liquids, and crucially, stay home from school and activities to prevent further transmission. If measles exposure is suspected, contact your healthcare provider in advance and request an isolation room visit to protect others.
The Broader Public Health Landscape: Challenges and Tools
The measles outbreak US is part of a larger, evolving public health narrative, presenting significant challenges that go beyond direct disease management.
Financial Burden of Outbreaks
Measles outbreaks carry a substantial financial burden. An average measles case can cost a health department approximately $43,000, with costs ranging from $7,000 to nearly $250,000 depending on the size and complexity of the outbreak. These costs stem from contact tracing, managing cases, implementing containment measures, and public health communications.
The Looming Threat to Elimination Status
The U.S. achieved measles elimination in 2000, meaning the disease was no longer continuously circulating domestically. However, the current surge puts this status at significant risk. The Americas region, for instance, lost its measles elimination status in November 2025 after Canada’s declaration. A final determination for the U.S. will be made in January 2026, considering whether continuous transmission occurred between January 2025 and January 2026. This assessment is complex, often requiring advanced genomic sequencing to differentiate new importations from ongoing domestic spread.
Critical Gaps in Health Communication and Policy
Public health experts have voiced significant concerns regarding federal health communication during this crisis. Limited public briefings and “mixed messages” from high-level officials can sow doubt and lead to public inaction, even among those not inherently anti-vaccine. Furthermore, policy shifts that modify recommended childhood immunization schedules, as seen with some vaccines being moved to “individual-based decision-making” or restricted to high-risk groups, are alarming to experts who warn they could “endanger the health of children.”
A Global “Perfect Storm”
Reduced U.S. funding for key global health organizations like USAID, GAVI, and the WHO poses a global threat. Experts predict these cuts will lead to more frequent and larger outbreaks of vaccine-preventable diseases worldwide, inevitably resulting in more frequent importations of these pathogens into the United States. This situation, combined with declining domestic vaccine coverage, creates what some describe as “a perfect storm brewing for the resurgence of vaccine-preventable diseases.”
New Tools for Tracking the Outbreak
In response to the need for more immediate and localized data, researchers from Johns Hopkins University, led by Farzin Ahmadi, PhD, launched a public county-level measles tracker on May 28, 2025. This innovative tool offers more granular, near-real-time data, updated twice weekly, in contrast to the CDC’s historical national and state-level weekly surveillance.
The tracker compiles information on vaccination status and age when reported by state and local health departments. It features interactive national maps showing cumulative and two-week county totals, distinguishing between imported and locally acquired cases. Users can also access tables, time-series graphs illustrating trends from 2018 through 2025, and epidemic curves for the most affected states. This resource is vital for both public health officials and the general public seeking detailed information on the evolving US measles outbreak.
Frequently Asked Questions
Why are measles cases surging in the US despite its elimination status?
Measles cases are surging in the US primarily due to a significant decline in childhood vaccination rates, especially among kindergartners, which has dropped below the critical 95% herd immunity threshold. Increased vaccine hesitancy, exacerbated during and after the COVID-19 pandemic, also plays a major role. Furthermore, a rise in global measles outbreaks means more imported cases into the U.S., infecting unvaccinated communities and threatening the nation’s measles elimination status achieved in 2000.
Where can I find real-time, county-level data on US measles outbreaks?
To find real-time, county-level data on US measles outbreaks, you can refer to the public measles tracker launched by Johns Hopkins University, led by Dr. Farzin Ahmadi, on May 28, 2025. This tracker provides twice-weekly updates of confirmed cases by county, offering more granular data than traditional national surveillance. It includes interactive maps, tables, and time-series graphs, distinguishing between imported and locally acquired cases, and summarizes vaccination status and age distributions when available.
Is the MMR vaccine truly safe and recommended for preventing measles?
Yes, the MMR (Measles, Mumps, Rubella) vaccine is widely considered safe and is strongly recommended by the CDC as the best way to prevent measles. It uses live, weakened viruses to provide immunity. Concerns about a link between the MMR vaccine and autism have been thoroughly debunked by numerous scientific studies involving millions of children over decades. Mild side effects like low-grade fever or rash are possible. The CDC recommends two doses: one at 12-15 months and another at 4-6 years, offering up to 99% protection.
Conclusion: Act Now to Protect Our Communities
The US measles outbreak of 2025 serves as a critical reminder of the fragility of public health achievements when vaccination rates decline. The highly contagious nature of measles, coupled with its severe potential complications and the significant costs of containment, demands immediate and informed action. The resurgence highlights the undeniable importance of the MMR vaccine not only for individual protection but for the collective health of our communities. By staying informed, adhering to recommended vaccination schedules, and supporting accurate public health communication, we can reverse this alarming trend and once again secure the health of all. Consult your healthcare provider to ensure your family’s immunizations are up-to-date.