Acute Myeloid Leukemia (AML) remains a formidable challenge in oncology, necessitating continuous innovation in treatment. For patients facing this aggressive blood cancer, the emergence of novel therapies offers renewed hope. Revumenib represents a significant leap forward, a targeted oral agent specifically designed to combat AML driven by certain genetic mutations. This comprehensive guide explores Revumenib’s mechanism, its efficacy in clinical trials, and its promising role in the evolving landscape of AML treatment, providing crucial insights for patients and healthcare professionals alike.
Understanding Acute Myeloid Leukemia (AML)
AML is a fast-growing cancer of the blood and bone marrow. It affects the myeloid cells, which are a type of white blood cell. This disease progresses rapidly, often requiring immediate and intensive treatment. The urgency arises from the rapid accumulation of abnormal cells, called blasts, in the bone marrow. These blasts interfere with the production of healthy blood cells, leading to severe complications like infections, anemia, and bleeding.
The Urgency of AML
Diagnosed in thousands each year, AML can strike at any age but is more common in older adults. Its aggressive nature means timely and effective intervention is critical for patient survival. Traditional therapies, while often effective initially, frequently lead to remission that can be short-lived, especially for patients with relapsed or refractory disease. This highlights the pressing need for new, more durable treatment options.
Current Treatment Landscape Challenges
Standard AML treatments typically involve intensive chemotherapy, sometimes followed by stem cell transplantation. While these approaches can achieve remission, many patients experience relapse. For individuals with relapsed or refractory AML (meaning the cancer returned or did not respond to initial treatment), options have historically been limited. Moreover, conventional chemotherapy can be associated with significant side effects, impacting quality of life. This underscores the demand for therapies that are both potent and precisely targeted.
Revumenib: A Targeted Approach to AML
Revumenib is a groundbreaking therapeutic agent. It operates as a menin-KMT2A (also known as MLL) inhibitor. This targeted action addresses specific genetic vulnerabilities in AML, a concept central to modern precision medicine. Its development marks a shift towards treatments that specifically attack the molecular drivers of cancer. This approach aims to maximize efficacy while potentially minimizing damage to healthy cells.
How Revumenib Works: The Menin-KMT2A Inhibition
At its core, Revumenib disrupts a critical interaction within leukemia cells. Many AML cases involve rearrangements or mutations of the KMT2A (MLL) gene or mutations in NPM1. These genetic alterations lead to abnormal protein interactions involving menin. Menin is a protein that collaborates with KMT2A to promote the uncontrolled growth of leukemia cells. Revumenib works by blocking the menin-KMT2A interaction. This blockade effectively disrupts the survival pathways of these specific leukemia cells, leading to their differentiation and death.
Targeting Specific Genetic Subtypes: KMT2A and NPM1
Revumenib’s power lies in its selectivity. It primarily targets AML patients whose cancer carries either a KMT2A rearrangement or an NPM1 mutation. These genetic markers are present in a significant subset of AML cases and are associated with poor prognoses. By focusing on these specific genetic drivers, Revumenib offers a highly personalized treatment strategy. This tailored approach represents a significant step forward in optimizing outcomes for patients with these challenging AML subtypes. Genetic testing is therefore paramount to identify eligible patients.
Clinical Efficacy and Trial Highlights
The potential of Revumenib has been rigorously evaluated in clinical trials. These studies have consistently demonstrated its promising activity in specific patient populations. The data collected provides crucial evidence of its ability to induce remission and improve patient outcomes.
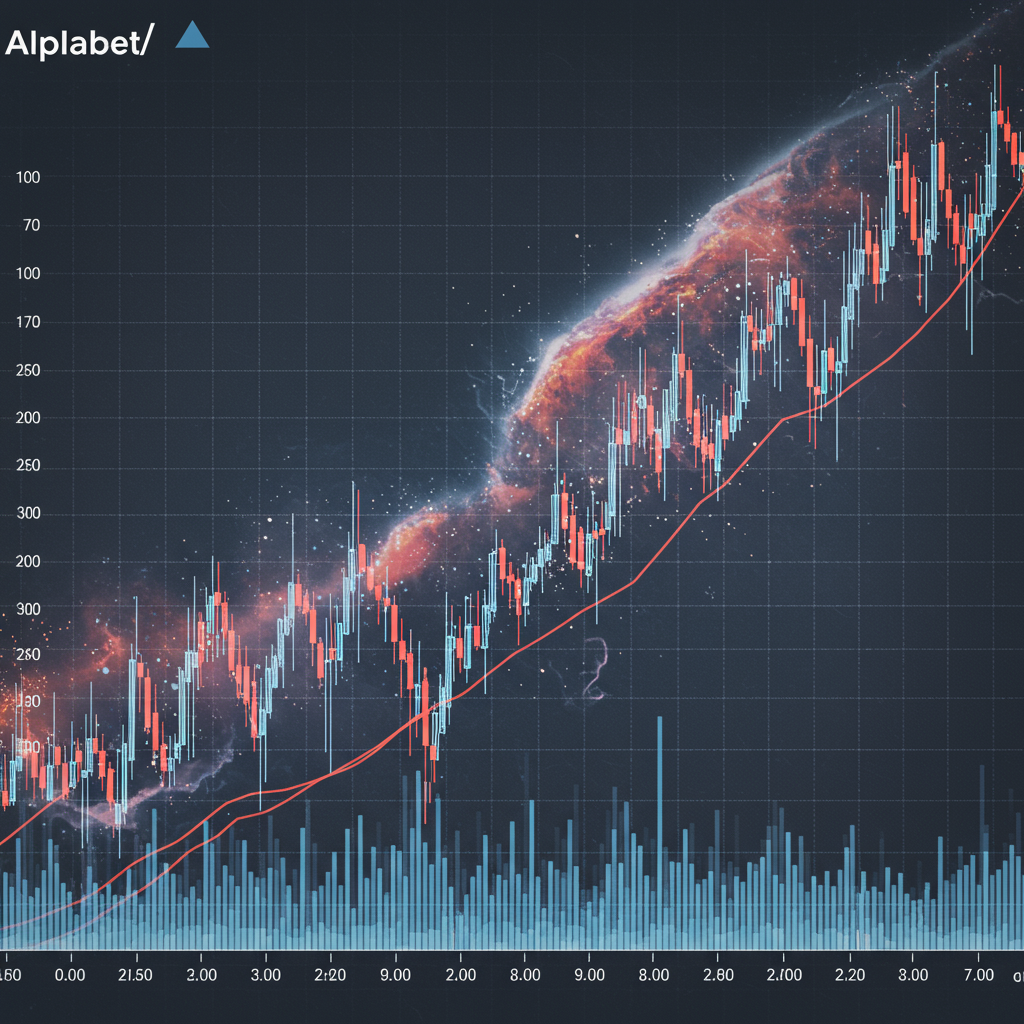
Key Findings from AUGMENT-101
The AUGMENT-101 clinical trial, a pivotal study, showcased Revumenib’s efficacy in patients with relapsed or refractory KMT2A-rearranged or NPM1-mutated AML. This Phase 2 trial reported significant response rates. Specifically, many patients achieved complete remission or complete remission with partial hematologic recovery. These remissions were often durable, indicating sustained disease control. The trial results have been highly anticipated within the hematology community, validating Revumenib’s mechanism of action and its potential to alter the treatment paradigm.
Real-World Impact and Patient Responses
Beyond trial statistics, the impact of Revumenib translates into tangible benefits for patients. Patients who had exhausted other treatment options found new hope. The responses observed were not just about measurable disease reduction; they often correlated with improved quality of life. This real-world effect is crucial for a disease as devastating as AML. The drug’s oral administration also offers a more convenient and less invasive treatment approach compared to intravenous chemotherapies, potentially enhancing patient adherence and overall experience.
Who is Revumenib For? Patient Selection
Identifying the right candidates for Revumenib treatment is crucial for maximizing its benefits. Its targeted nature means that patient selection relies heavily on specific genetic markers. This emphasizes the growing importance of precision medicine in oncology.
Relapsed/Refractory AML
Revumenib is primarily indicated for patients with relapsed or refractory AML. These are individuals whose disease has returned after initial treatment or has not responded to previous therapies. For this difficult-to-treat population, novel agents like Revumenib offer a lifeline. It provides a much-needed option where traditional treatments have failed, potentially extending survival and improving the prospects for further therapeutic interventions.
Biomarker Testing: A Crucial Step
Before considering Revumenib, patients must undergo comprehensive genetic testing. This testing identifies the presence of KMT2A rearrangements or NPM1 mutations in their leukemia cells. These biomarkers are the gatekeepers to Revumenib eligibility. Without these specific genetic alterations, the drug is unlikely to be effective. Consequently, integrating advanced molecular diagnostics into the routine AML diagnostic pathway becomes indispensable for optimal treatment planning. This ensures that the right patients receive the right therapy.
Potential Side Effects and Management
Like all powerful medications, Revumenib can cause side effects. Understanding and managing these adverse events is essential for patient safety and treatment adherence. Healthcare providers play a critical role in monitoring patients and implementing supportive care strategies.
Common Adverse Events
Clinical trials have detailed the side effect profile of Revumenib. Common adverse events include differentiation syndrome, QTc prolongation, and gastrointestinal issues like nausea and diarrhea. Differentiation syndrome is a potentially serious complication specific to targeted therapies like Revumenib. It requires careful monitoring and prompt management. Symptoms can include fever, weight gain, respiratory distress, and fluid retention.
Mitigating Risks for Better Outcomes
Effective management of side effects is paramount. For differentiation syndrome, early recognition and treatment with corticosteroids are vital. Regular electrocardiograms (ECGs) are necessary to monitor for QTc prolongation, and electrolyte imbalances must be corrected. Proactive antiemetic and antidiarrheal medications can help manage gastrointestinal symptoms. Close collaboration between patients and their healthcare teams ensures that side effects are addressed swiftly, allowing patients to continue treatment with greater comfort and safety. This proactive approach helps optimize treatment outcomes and enhances patient quality of life.
The Future Landscape of AML Treatment
Revumenib’s arrival marks a pivotal moment in AML therapy. Its success paves the way for further research and the development of even more sophisticated treatments. The future of AML treatment is increasingly focused on precision and combination approaches.
Revumenib’s Role in Combination Therapies
Current research is actively exploring Revumenib in combination with other AML agents. Combining Revumenib with chemotherapy or other targeted therapies could potentially enhance its efficacy. These combination strategies aim to overcome resistance mechanisms and achieve deeper, more durable remissions. Early studies suggest that such synergistic approaches could become the new standard, particularly for patients with complex disease profiles. This involves careful trial design to identify the most effective and tolerable drug combinations.
Ongoing Research and Next-Generation Treatments
The success of menin-KMT2A inhibitors like Revumenib fuels ongoing research into other novel targets. Scientists are investigating new pathways and developing next-generation drugs to treat AML. This includes exploring therapies for other genetic subtypes and refining existing treatments. The ultimate goal is to offer a personalized and curative approach for every AML patient. This continuous evolution of therapies promises a brighter future for those affected by this challenging disease.
Frequently Asked Questions
What makes Revumenib different from traditional AML treatments?
Revumenib stands out as a highly targeted oral therapy, contrasting with traditional intensive chemotherapy. It specifically inhibits the menin-KMT2A interaction, which is a key driver of leukemia cell growth in AML patients with KMT2A rearrangements or NPM1 mutations. Traditional treatments often use broad-acting cytotoxic agents. Revumenib’s precision means it primarily affects cancer cells with these specific genetic alterations, potentially leading to fewer side effects on healthy tissues compared to conventional chemotherapy. This targeted approach offers a personalized treatment option for a specific subset of AML patients.
How do doctors determine if Revumenib is a suitable treatment option for a patient?
Doctors determine Revumenib suitability through comprehensive genetic testing of a patient’s leukemia cells. This essential biomarker testing identifies the presence of KMT2A rearrangements or NPM1 mutations. If these specific genetic alterations are found, and the patient has relapsed or refractory AML, Revumenib may be considered. Healthcare providers also assess the patient’s overall health, prior treatment history, and ability to manage potential side effects. This careful diagnostic and evaluative process ensures that the therapy is appropriately matched to the patient’s unique cancer profile.
What are the primary benefits and considerations for patients prescribed Revumenib?
The primary benefit of Revumenib is its potential to induce significant and durable remissions in patients with relapsed or refractory KMT2A-rearranged or NPM1-mutated AML, a group with limited options. It offers a targeted, oral therapy, which can be more convenient than intravenous treatments. Key considerations include the need for specific genetic mutations for efficacy and the potential for side effects like differentiation syndrome, QTc prolongation, and gastrointestinal issues. Patients must be diligently monitored by their healthcare team, and active management of adverse events is crucial to ensure safety and maintain treatment adherence for optimal outcomes.
Conclusion
Revumenib represents a beacon of hope for patients battling relapsed or refractory Acute Myeloid Leukemia, particularly those with specific genetic mutations. Its innovative mechanism of action, precisely targeting the menin-KMT2A interaction, showcases the power of personalized medicine. Clinical trials have demonstrated its significant efficacy, offering a new pathway to remission and improved quality of life. As research continues, exploring combination therapies and next-generation treatments, Revumenib’s role will undoubtedly evolve. For patients and clinicians alike, it underscores a future where AML treatment is increasingly precise, effective, and tailored to the individual’s unique genetic fingerprint.