The United States is facing an urgent public health crisis. measles cases have surged to levels not seen since the highly contagious disease was declared eliminated in the year 2000. This alarming rise threatens the country’s long-held status and highlights critical vulnerabilities in vaccination coverage. As of early July 2025, over 1,277 cases have been reported nationwide, according to health officials tracking the spread. Tragically, this resurgence has already resulted in the first measles deaths in a decade, underscoring the virus’s dangerous potential.
The current situation is largely fueled by significant outbreaks, primarily centered in the Southwest. Declining vaccination rates, fueled in part by persistent misinformation, are creating pockets of vulnerability where measles can easily spread. Experts warn that without swift and effective intervention, the U.S. risks losing its measles elimination status altogether.
A Threat to Elimination Status
Measles was officially eliminated in the United States in 2000. This meant the disease was no longer continuously spreading within the country for a full year. The elimination was a major public health achievement, made possible by widespread vaccination efforts.
However, “elimination” does not mean the disease is gone forever. Cases can still be imported by travelers returning from other countries where measles is more common. When these imported cases enter communities with low vaccination rates, large outbreaks can occur. If measles transmission continues uninterrupted for 12 months or more across the U.S., the country would lose its elimination status. This current surge puts that milestone achievement at serious risk.
The Epicenter of the Outbreak
A major driver of the recent case spike is a large outbreak that began in a community in West Texas. Gaines County, located in this region, became the epicenter. Health data reveals concerningly low vaccination rates among children in this area.
For the 2023-24 school year, only 82% of kindergarteners in Gaines County had received the recommended two doses of the Measles, Mumps, and Rubella (MMR) vaccine. This rate falls significantly below the 95% coverage needed for herd immunity. Herd immunity protects vulnerable individuals, like infants too young to be vaccinated or those with compromised immune systems. The low coverage in Gaines County created fertile ground for the virus to take hold and spread rapidly.
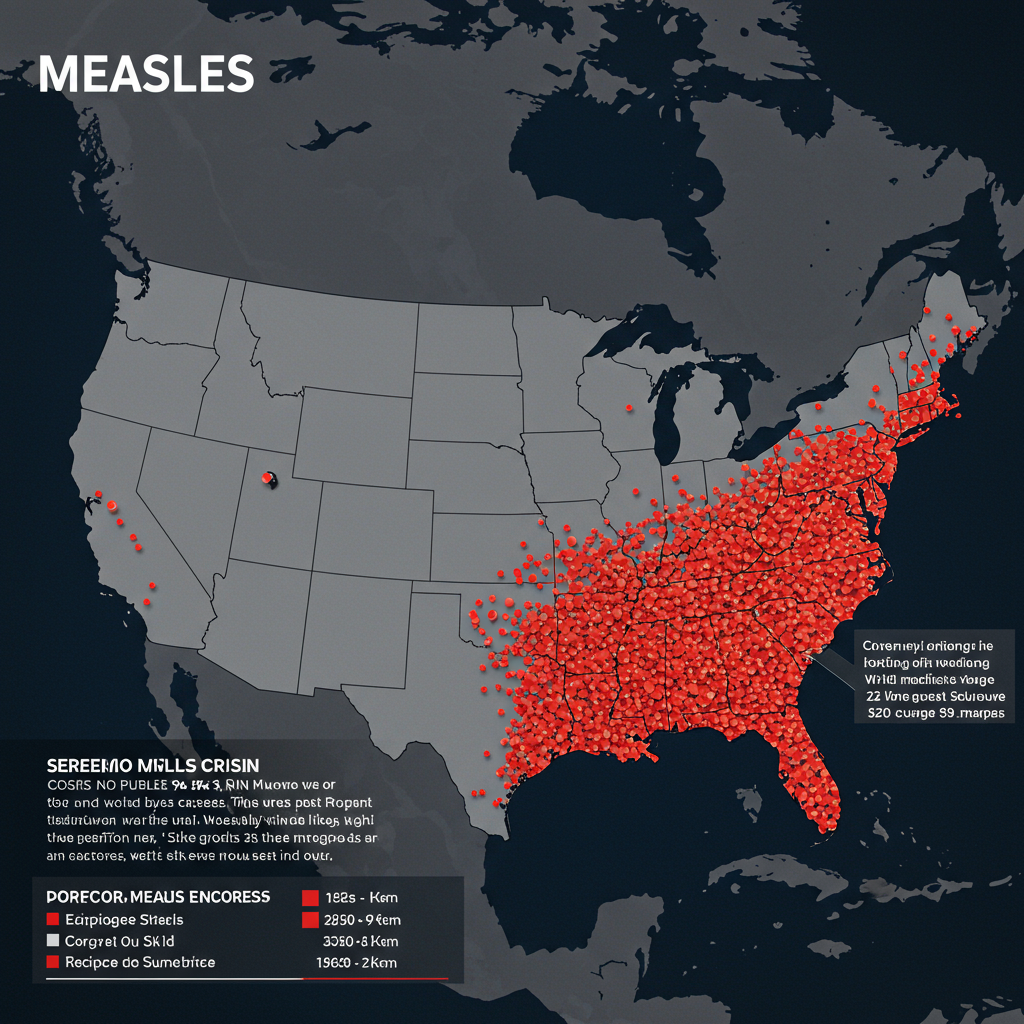
Spreading Beyond the Initial Cluster
While West Texas saw the largest concentration of cases, with over 700 reported in Texas alone, the outbreak has not remained isolated. The virus has spread to several other states. Additionally, numerous smaller outbreaks, often linked to international travel, have been detected in various locations across the country.
This widespread geographic impact highlights the ease with which measles can travel in today’s connected world. Any community with insufficient vaccination coverage is potentially vulnerable to an imported case igniting an outbreak. The current landscape of fragmented outbreaks across multiple states underscores the national scope of the problem.
Why Are Cases Rising? Key Factors
Multiple factors contribute to the disturbing rise in measles cases. A significant issue is the nationwide decline in childhood vaccination rates. National data shows that the proportion of kindergarteners receiving the two-dose MMR vaccine has dipped below 93% in the 2023-24 school year. This is down from a rate of over 95% just a few years prior, in the 2019-20 school year.
This erosion of vaccination coverage creates a larger pool of susceptible individuals. The more unvaccinated people there are, the easier it is for measles to spread from one person to another, leading to larger and longer-lasting outbreaks. The 2019 outbreak, which saw 1,274 cases, also occurred in communities with low vaccination rates, serving as a stark precedent.
The Impact of Misinformation
Adding complexity to the public health response is the pervasive spread of misinformation about vaccines. Despite overwhelming scientific evidence confirming the safety and effectiveness of the MMR vaccine, false claims continue to circulate. Some messages frame vaccination purely as a personal choice, downplay the risks of measles, or promote unproven alternative treatments.
Health care providers on the front lines report that countering this misinformation is a significant challenge. Some patients have opted for unproven methods, such as relying solely on vitamin A, instead of getting vaccinated. While vitamin A can be administered under medical supervision for support in measles cases, it is not a substitute for vaccination and is not a treatment for the disease itself. This underscores how false narratives can directly impede effective public health measures.
Funding Challenges for Response Efforts
Responding to measles outbreaks is also resource-intensive. Public health officials note that addressing each individual measles case can cost tens of thousands of dollars. These costs add up quickly during large outbreaks. Compounding this challenge are recent funding limitations impacting state health departments.
Significant cuts to public health funding, including money previously available through COVID-19 response grants, have reduced the resources available for outbreak containment efforts. This leaves health departments with fewer personnel and less flexibility to conduct the intensive contact tracing, public messaging, and vaccination campaigns needed to stop the spread of highly infectious diseases like measles.
Understanding Measles: Symptoms and Dangers
Measles is far more serious than just a rash. It is a highly contagious respiratory illness caused by a virus. The initial symptoms often include a high fever, cough, runny nose, and red, watery eyes (conjunctivitis). A distinctive sign is the appearance of tiny white spots, known as Koplik spots, inside the mouth near the molars.
Within a few days, a characteristic blotchy red rash erupts, typically starting on the face and spreading downwards across the body. Measles is incredibly contagious; the virus can linger in the air and on surfaces for up to two hours after an infected person leaves a room. An infected person can spread measles from four days before the rash appears through four days after.
Severe Complications and Fatalities
While many people recover from measles, it can lead to severe complications, especially in young children, pregnant women, and individuals with weakened immune systems. Serious complications can include pneumonia, encephalitis (swelling of the brain), ear infections, and severe diarrhea.
Globally, measles remains a leading cause of death among young children. In the U.S., even with advanced medical care, the risk of death is real. According to the CDC, approximately 1 to 3 out of every 1,000 children who contract measles die from respiratory or neurological complications. The recent deaths of three unvaccinated individuals in Texas and New Mexico tragically confirm this risk.
The Proven Solution: Vaccination
Fortunately, measles is a preventable disease thanks to a highly effective vaccine. The MMR vaccine protects against measles, mumps, and rubella. Two doses of the MMR vaccine are 97% effective at preventing measles and provide lifelong protection for most people.
The standard recommendation is for children to receive their first dose between 12 and 15 months of age and the second dose between 4 and 6 years old. However, in areas experiencing outbreaks, health officials may recommend an early dose for infants aged 6 to 11 months. For unvaccinated children over 12 months, the guidance is typically one dose followed by a second dose at least 28 days later.
Vaccination is not just about individual protection; it’s about community protection. High vaccination rates create herd immunity, making it difficult for the virus to circulate and protecting those who cannot be vaccinated. Public health experts emphasize that widespread vaccination is the most critical strategy to halt the current surge and prevent future outbreaks.
Fighting Back Against the Virus
Public health agencies are working to contain the spread, often modeling their efforts on past successful campaigns. The response to the 2019 outbreak in New York, which involved a vaccine mandate in affected areas and administering tens of thousands of doses, is seen as a successful model. However, applying such strategies faces challenges related to funding and overcoming vaccine hesitancy fueled by misinformation.
Experts continue to stress the importance of clear, accurate communication about vaccine safety and effectiveness. Countering false narratives requires consistent efforts from health officials, medical professionals, and trusted community leaders. Rebuilding public trust and addressing vaccine gaps are essential steps in bringing the current outbreak under control and preventing measles from re-establishing itself in the U.S.
Frequently Asked Questions
What are the latest measles case numbers and where is the main outbreak occurring?
As of early July 2025, the United States has reported over 1,277 measles cases nationwide. This is the highest total since the disease was eliminated in 2000. The largest current outbreak originated in a community in West Texas, particularly in Gaines County, which has low local vaccination rates. The outbreak has since spread to other states.
How can someone get information about measles symptoms or the MMR vaccine?
Reliable information about measles symptoms, risks, and the MMR vaccine is available from trusted public health sources. The Centers for Disease Control and Prevention (CDC) website is a primary resource. You can also consult with your local health department or a healthcare provider, such as a pediatrician, for accurate information and guidance on vaccination.
Why is getting vaccinated against measles important now, especially for children?
Vaccination is critical because measles is highly contagious and can cause severe complications, including pneumonia, brain damage, and death. The MMR vaccine is 97% effective after two doses. High vaccination rates protect not only vaccinated individuals but also vulnerable people in the community, like infants or those with weakened immune systems, by creating herd immunity. The current surge in cases demonstrates the real danger of low vaccination rates.
Conclusion
The resurgence of measles in the United States to levels not seen in a quarter-century is a grave reminder of the importance of maintaining high vaccination rates. The current outbreaks, particularly driven by low coverage in areas like West Texas, highlight how quickly a preventable disease can return when communities become vulnerable. Addressing declining national vaccination rates, combating misinformation, and ensuring adequate public health funding are essential steps. Protecting the U.S. from losing its measles elimination status requires a collective effort to ensure everyone who can be vaccinated receives their recommended doses, securing community immunity and preventing future tragic outcomes.