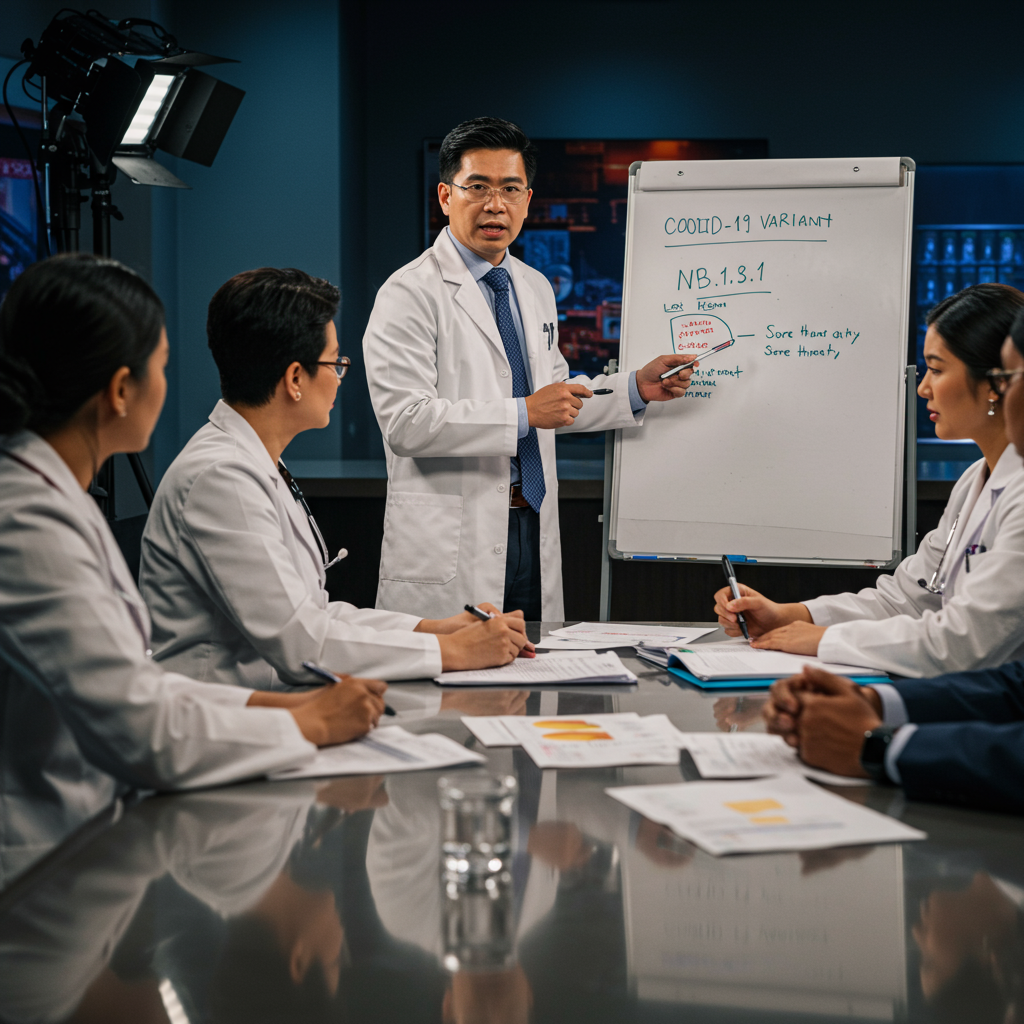
A new variant of covid-19 is gaining attention, partly due to a startling nickname: “Razor Blade throat.” This moniker reflects a particularly severe sore throat symptom reported by some individuals infected with the variant officially known as NB.1.8.1. While headlines about rising cases and painful symptoms can sound alarming, medical experts emphasize key information about this variant and how to protect yourself. Understanding the facts can help navigate concerns and maintain health this summer.
What is “Razor Blade Throat”? Understanding the Symptom
The vivid nickname “Razor Blade Throat” comes directly from patient descriptions. Some individuals have reported experiencing a sore throat so intense it feels like swallowing glass or razor blades. This symptom is particularly associated with the NB.1.8.1 variant, also nicknamed “Nimbus,” which is currently circulating widely.
Despite the dramatic name, medical experts like Dr. Jacob Wood, a Family Medicine physician, and national experts such as Dr. William Schaffner and Dr. Carrie Horn, state this symptom is not entirely new. A very painful sore throat has been a possible COVID-19 symptom throughout the pandemic. Studies indicate a sore throat occurs in a significant percentage of COVID cases, sometimes reported as high as 70%. Experts suggest that while NB.1.8.1 may be associated with a painful sore throat for some, it doesn’t necessarily represent a fundamental shift in symptom severity compared to previous variants. It may simply be a symptom that is currently receiving more public attention as the variant spreads.
Introducing the NB.1.8.1 Variant (Nimbus)
The variant behind the “Razor Blade Throat” reports is officially designated NB.1.8.1. The World Health Organization (WHO) is currently monitoring NB.1.8.1, classifying it as a “variant under monitoring.” This classification means it warrants attention but is not currently considered a higher-risk “variant of interest” or “variant of concern.”
First detected in China in January, NB.1.8.1 is a descendant of the Omicron variant, specifically evolving from the recombinant lineage XVD.1.5.1. It has since spread across Asia, Europe, and into the United States. National data from the Centers for Disease Control and Prevention (CDC) shows NB.1.8.1 has rapidly become one of the most common variants circulating. As of early June, estimates suggest it accounted for roughly 37-38% of all COVID-19 cases nationwide, nearly equaling the dominant LP.8.1 variant. Regional data in places like California indicate an even higher prevalence, projected at 55% in some areas by May.
Transmissibility vs. Severity: What Experts Know
Some experts, like Professor Subhash Verma, describe NB.1.8.1 as a “slightly upgraded version” of LP.8.1. There are suggestions that this variant may be more easily transmitted. Changes in the virus’s spike protein may allow it to attach more readily to human cells. It might also be slightly more effective at evading antibodies from past infections or vaccination compared to some previous strains. This increased transmissibility likely contributes to its rapid spread.
However, despite its growing prevalence and potential for easier transmission, experts currently find no clear evidence that NB.1.8.1 causes more severe illness. National data indicates that hospitalization rates have remained stable so far, even as this variant has become dominant. Experts caution that individuals in high-risk groups, such as older adults or those with underlying conditions, remain vulnerable to severe outcomes if infected.
Beyond Sore Throat: Recognizing NB.1.8.1 Symptoms
While the painful sore throat has captured attention, NB.1.8.1 typically presents as a classic upper respiratory illness. The CDC lists a wide range of potential COVID-19 symptoms. These are generally consistent across circulating variants, including NB.1.8.1.
Common symptoms can include:
Runny nose
Nasal congestion
Cough
Body aches and muscle pain
Fatigue
Headache
Fever or chills
Shortness of breath or difficulty breathing
Loss of taste or smell (less common with newer variants)
Nausea or vomiting
Experiencing a sore throat, even a severe one, does not automatically mean you have NB.1.8.1. Other illnesses like strep throat or the flu also cause sore throats. Local doctors emphasize that a fever could be a key indicator. If you have a bad sore throat accompanied by a fever, seeking medical evaluation is wise to determine the cause.
Protecting Yourself: Practical Prevention Steps
Protecting yourself from NB.1.8.1 and other respiratory illnesses involves familiar public health measures. These actions are effective and easy to implement in daily life.
Key protective steps include:
Wash your hands frequently and thoroughly with soap and water.
Use hand sanitizer when washing is not possible.
Avoid close contact with individuals who are known to be sick.
Consider wearing a mask in crowded indoor settings, especially if you are at higher risk.
Increase ventilation indoors by opening windows or using air purifiers.
Stay home if you feel unwell to prevent spreading germs.
Ensure adequate hydration by drinking plenty of fluids like water and herbal teas.
Testing is also an important tool. If you develop symptoms, getting tested for COVID-19 can help confirm the diagnosis and guide treatment decisions. Rapid tests are widely available and can provide quick results.
The Role of Vaccination Amidst Policy Changes
Vaccination remains a critical tool in reducing the risk of severe illness, hospitalization, and death from COVID-19, including variants like NB.1.8.1. Experts worldwide expect current vaccines to remain effective against NB.1.8.1 for preventing symptomatic disease and severe outcomes. The CDC recommends that individuals aged 6 months and older stay up-to-date with the latest COVID-19 vaccines, specifically the 2024-2025 formulation. High-risk groups are particularly encouraged to get vaccinated.
However, navigating vaccine recommendations has become more complex recently. Controversial changes in federal policy have removed the COVID-19 vaccine from recommended immunization schedules for healthy children and healthy pregnant women. Additionally, regulatory processes for future boosters for younger adults are changing. These actions have drawn strong criticism from medical professional organizations and state/local health officials. Critics worry these changes could make vaccine access more difficult and expensive for some Americans and erode public trust in health guidance. Despite these federal shifts, many state and local health departments continue to recommend access to authorized vaccines for all eligible individuals. It’s important to consult with your healthcare provider about the best vaccination strategy for you and your family. Note that updated vaccines targeting circulating strains like NB.1.8.1 are different from traditional “booster shots,” which were additional doses of the same formula.
Managing Symptoms and When to Seek Help
If you test positive for COVID-19, even if symptoms seem mild or typical of an upper respiratory illness, managing symptoms and monitoring your health is important. For symptom relief, over-the-counter medications like ibuprofen or acetaminophen can help reduce fever and body aches (always follow package directions and consult a doctor if unsure). Staying well-hydrated is essential, especially with a painful sore throat, as dehydration can worsen discomfort.
For individuals at high risk of severe COVID-19, contacting a healthcare provider after a positive test is crucial. Antiviral treatments are available that can significantly reduce the risk of severe outcomes if started early. Even for lower-risk individuals, consulting a doctor is advised if symptoms worsen or if you experience warning signs. Seek immediate medical care for symptoms such as trouble breathing, persistent chest pain or pressure, new confusion, or inability to stay awake.
Frequently Asked Questions
What is the NB.1.8.1 COVID variant causing “Razor Blade Throat”?
NB.1.8.1 is a new COVID-19 variant, also nicknamed “Nimbus,” that is currently widespread in the U.S. It’s an Omicron descendant and is being monitored by the WHO. The nickname “Razor Blade Throat” comes from reports of some infected individuals experiencing a particularly painful sore throat. Experts say this symptom isn’t entirely new but is part of the known range of COVID symptoms.
Where is the NB.1.8.1 variant most prevalent in the US?
As of early June, CDC data estimated NB.1.8.1 accounted for roughly 37-38% of US COVID cases, making it the second most dominant variant nationally. Regional data, like in California, showed even higher prevalence rates, exceeding 50% in some areas. Local doctors in places like Baton Rouge, Louisiana, note they are starting to see cases appear, although local numbers may lag behind national trends.
Should I get a COVID vaccine to protect against the NB.1.8.1 variant?
Yes, medical experts recommend staying up-to-date with the latest COVID-19 vaccines, such as the 2024-2025 formulation, to protect against current circulating variants like NB.1.8.1. While recent federal policy changes have altered recommendations for some groups (healthy children, healthy pregnant women), most health organizations and state health departments still recommend access to authorized vaccines for eligible individuals due to their effectiveness against severe disease. Consult your doctor about which vaccine is right for you.
Staying Informed and Prepared
While the nickname “Razor Blade Throat” might sound frightening, experts emphasize that the NB.1.8.1 variant primarily causes symptoms similar to other recent COVID-19 strains. It does not appear to be causing more severe illness overall* at this time, though its increased transmissibility means more people could become infected. The landscape of COVID-19 public health guidance is experiencing shifts due to policy changes, adding complexity for the public. Staying informed about the latest variant information, practicing proven prevention methods, getting vaccinated according to expert advice, and knowing when to seek medical attention are the best strategies to protect yourself and your community. COVID-19 is still a serious infection, not just a common cold, with potential risks including long COVID, underscoring the importance of continued vigilance.
References
- www.wafb.com
- abcnews.go.com
- www.latimes.com
- <a href="https://www.huffpost.com/entry/people-are-reporting-a-frightening-covid-symptom-right-now-heres-what-to-know-googl685d64c3e4b0bd0253106e62″>www.huffpost.com
- www.usatoday.com