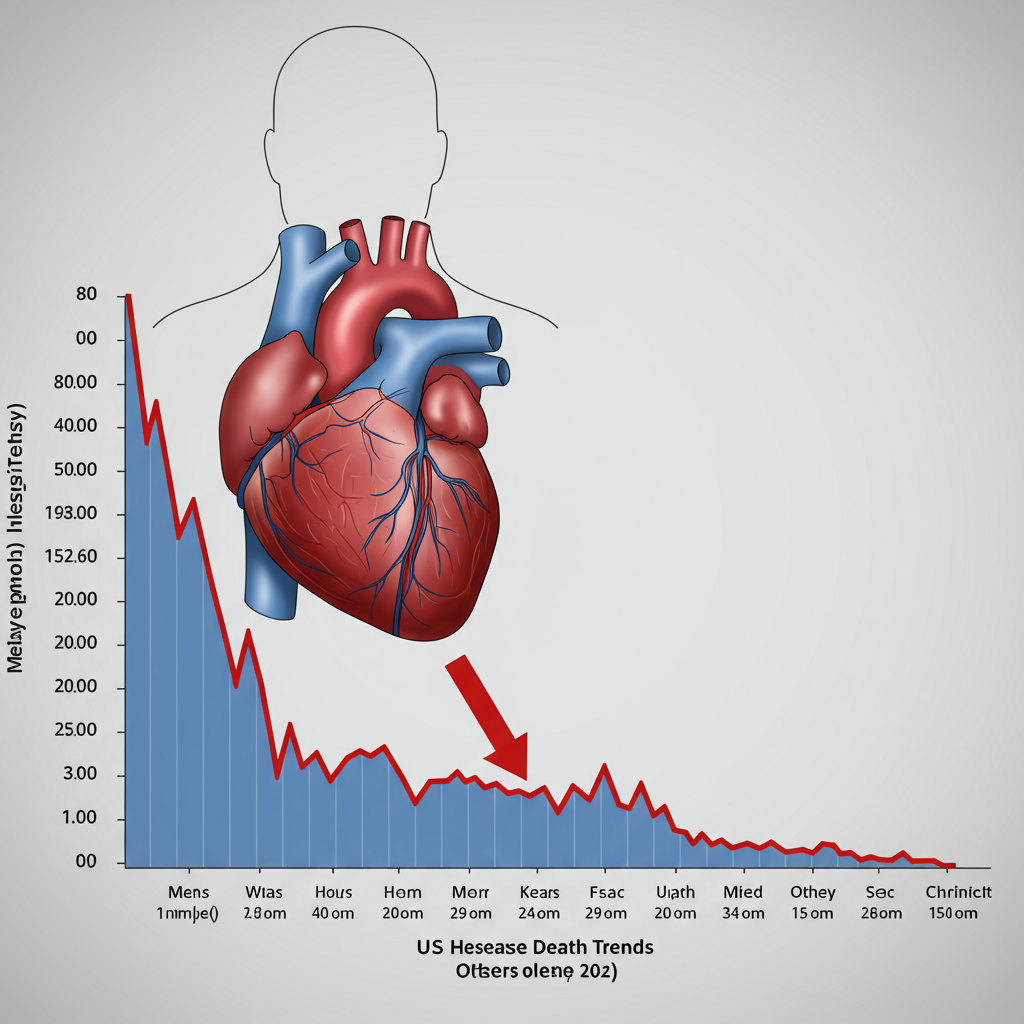
heart disease remains the leading cause of death in the United States, claiming a life approximately every 33 seconds. However, a significant shift has occurred over the past five decades in how Americans are dying from heart-related issues. While dramatic progress has been made in preventing death from heart attacks, fatalities linked to other chronic heart conditions are now on the rise, presenting a new challenge for public health.
This changing landscape is detailed in a recent report published in the Journal of the American Heart Association. The study analyzed nationwide mortality data spanning from 1970 to 2022, revealing both remarkable successes and emerging concerns in the fight against cardiovascular disease. Understanding this trend is crucial for individuals and healthcare providers alike to focus prevention and management efforts effectively.
Heart Attack deaths Plummet Over 50 Years
One of the most striking findings of the report is the dramatic reduction in deaths specifically attributed to acute myocardial infarctions, commonly known as heart attacks. Fatalities from heart attacks saw a remarkable decrease of nearly 90% between 1970 and 2022.
In 1970, heart attacks were responsible for more than half of all heart disease deaths in the U.S. By 2022, that proportion had fallen to less than one-third. This success story didn’t happen by accident. It’s the result of decades of advancements in medical science, public health initiatives, and emergency care.
Why Are Fewer People Dying from Heart Attacks?
Experts point to several key factors behind the impressive decline in heart attack mortality. Improvements span prevention, diagnosis, and treatment.
Major medical breakthroughs have played a critical role. These include the widespread availability of bystander CPR and portable defibrillators, improved coronary care units, and significant progress in cardiac imaging techniques like angiography. Procedures such as coronary artery bypass surgery, balloon angioplasty, and coronary stenting have become standard practice, effectively restoring blood flow during an attack.
Furthermore, the development and widespread use of potent medications like aspirin, antiplatelet therapies, and statins have significantly improved outcomes. Faster emergency response times and the recognition of heart attacks as emergencies requiring rapid intervention (ideally within 90 minutes) have also been life-saving. Dr. Michael G. Nanna, an interventional cardiologist, described this decline as a “remarkable public health success.”
Public health campaigns have also contributed by focusing on major risk factors. Efforts initiated decades ago, like campaigns against tobacco smoking, helped reduce the prevalence of this significant cardiovascular risk factor. Overall, these combined efforts have transformed heart attacks from what was often a “death sentence” in the past into a condition that is increasingly survivable.
The Rise of Other Heart-Related Fatalities
While the news about heart attack survival is positive, the report highlights a concerning counter-trend. As deaths from acute events like heart attacks have fallen, fatalities from other chronic forms of heart disease have concurrently increased.
Over the same 1970-2022 period, the age-adjusted death rate from non-heart attack related heart conditions collectively rose by 81%. In 1970, these conditions accounted for a small fraction (9%) of all heart disease deaths. By 2022, they were responsible for a substantial 47% of heart disease fatalities.
Specific Conditions Seeing Increased Deaths
The study identified several specific heart conditions driving this increase in non-heart attack deaths:
Heart Failure: Deaths from heart failure have more than doubled, increasing by 146%.
Hypertension-Related Heart Disease: Fatalities linked to high blood pressure also more than doubled, rising by 106%.
Arrhythmias: Deaths caused by abnormal heart rhythms saw the most dramatic percentage increase, surging by a staggering 450%.
This shift means that while the overall rate of heart disease deaths has decreased by 66% since 1970, the type of heart disease that is fatal is changing significantly.
Why Are Deaths from Other Conditions Rising?
The increase in deaths from conditions like heart failure, hypertension, and arrhythmias is complex, influenced by several interconnected factors.
One primary reason is the success in treating heart attacks themselves. As more people survive acute heart attacks, they live longer, but their hearts may have been weakened or damaged. This damage can lead to chronic conditions such as heart failure or increase the risk of dangerous arrhythmias later in life. Dr. Cheng-Han Chen, a cardiologist, notes that surviving a heart attack often serves as a “catalyst” for long-term chronic heart conditions.
Impact of an Aging Population and Rising Risk Factors
Another significant factor is the aging of the U.S. population. Average life expectancy increased from around 71 years in 1970 to 77.5 years in 2022. Since heart failure, hypertension, and arrhythmias are conditions strongly associated with age, living longer increases the likelihood of developing and eventually succumbing to these issues.
Furthermore, the prevalence of major cardiovascular risk factors has increased over the past few decades. Experts like Dr. Sarraju point out that rising rates of obesity, type 2 diabetes, and high blood pressure in the population contribute significantly to the increasing burden of chronic heart conditions. Sedentary lifestyles and poor dietary habits characterized by processed and fast food also play a major role.
Societal stressors and socioeconomic issues can further complicate lifestyle risk factors, making prevention and management more challenging for many people. Specific factors like pregnancy complications, such as hypertension or gestational diabetes, also increase a woman’s lifetime risk of heart disease.
Focus on Heart Failure and Arrhythmias
Heart failure means the heart isn’t pumping blood as efficiently as it should. It exists on a spectrum, ranging from mild forms that may not significantly impact lifespan with proper management to severe cases. Surviving a heart attack, especially a major one, can cause lasting damage to the heart muscle, increasing the risk of developing heart failure.
Arrhythmias, or abnormal heart rhythms, can range from harmless to life-threatening. The dramatic 450% increase in arrhythmia-related deaths highlights this as an area of growing concern. Arrhythmias include slow heart rates (bradycardia), fast rates (tachycardia), and irregular beats like atrial fibrillation (a type of supraventricular arrhythmia) or dangerous ventricular arrhythmias.
While many arrhythmias are benign, severe ones can compromise blood flow to vital organs, potentially causing fatal outcomes. Reducing the risk of arrhythmias is particularly crucial for heart attack survivors, as irregular rhythms, especially ventricular ones, can be life-threatening.
Taking Action: Prevention and Management
The changing landscape of heart disease mortality underscores the ongoing need for robust prevention strategies and effective management of chronic conditions. While medical advancements have been revolutionary in treating acute events, the focus must now expand to help people age with healthier hearts and better manage long-term issues.
Regular medical checkups are essential, including evaluations of heart health risk factors like blood pressure, cholesterol, and blood sugar. If you experience symptoms like your heart beating irregularly, it’s important to consult a doctor for evaluation.
For individuals who have survived a heart attack or been diagnosed with chronic heart conditions like heart failure or arrhythmias, adhering to medical advice and prescribed treatments is vital. This can include specific medication regimens, cardiac rehabilitation programs, devices like implantable defibrillators, and management of co-occurring conditions like sleep apnea.
Lifestyle modifications remain the cornerstone of heart health, both for preventing disease and managing existing conditions.
AHA’s Essential Eight for Heart Health
The American Heart Association (AHA) provides a clear framework for maintaining cardiovascular wellness. Their “Essential Eight” list includes:
Eating healthy foods
Being more physically active
Quitting tobacco use
Getting healthy sleep
Managing body weight
Controlling cholesterol levels
Regulating blood sugar
- Managing blood pressure
- www.healthline.com
- www.everydayhealth.com
- med.stanford.edu
- newsroom.heart.org
- www.aarp.org
It’s never too late to adopt healthier habits. Even small changes can significantly impact your long-term heart health and reduce your risk of developing or worsening chronic conditions that are increasingly contributing to heart disease deaths. Engaging proactively with healthcare providers is key to monitoring risk factors and managing existing heart ailments effectively.
Frequently Asked Questions
Why are fewer Americans dying from heart attacks now compared to 50 years ago, but deaths from other heart issues are increasing?
Fewer people are dying from heart attacks primarily due to major advancements in emergency medical treatment, life-saving procedures like stenting, and effective medications developed over the past five decades. However, as more people survive heart attacks, they may develop chronic heart conditions later in life due to heart damage. Combined with an aging population and rising rates of risk factors like obesity and diabetes, this has led to an increase in deaths from conditions like heart failure, hypertension-related heart disease, and arrhythmias.
What specific heart conditions are causing more deaths now than heart attacks used to?
While heart attacks were once the leading cause of heart-related death, fatalities from other conditions are now more common. The recent study highlights significant increases in deaths from heart failure (up 146%), hypertension-related heart disease (up 106%), and particularly arrhythmias (up 450%) between 1970 and 2022. These chronic conditions now account for a much larger proportion of overall heart disease deaths.
What can individuals do to protect themselves from the types of heart conditions that are on the rise?
Protecting yourself involves a focus on prevention and managing risk factors. This includes adopting healthy lifestyle habits recommended by organizations like the AHA, such as eating a balanced diet, exercising regularly, maintaining a healthy weight, quitting smoking, getting adequate sleep, and managing stress. It’s also crucial to get regular medical checkups to monitor and control blood pressure, cholesterol, and blood sugar levels. For those with existing heart conditions, diligent management and following medical advice are essential.
Conclusion
The data clearly shows a critical evolution in the landscape of heart disease mortality in the U.S. The dramatic success in reducing heart attack deaths is a testament to decades of medical innovation and public health effort. However, the concurrent rise in deaths from chronic conditions like heart failure, hypertension, and arrhythmias underscores that the fight against heart disease is far from over. Addressing these emerging challenges requires a renewed focus on preventing risk factors, promoting healthy aging, and providing comprehensive, long-term care for chronic cardiovascular issues. By understanding this shift, individuals and the healthcare system can better target efforts to improve heart health outcomes for future generations.