Gut health is fundamental to overall well-being, yet digestive problems are becoming increasingly prevalent across the United States. Estimates suggest that a significant portion of the population, potentially up to two-thirds of Americans, grapples with some form of gut-related issue. This growing trend is a cause for concern among medical professionals who observe a potential rise in specific conditions, including Irritable Bowel Syndrome (IBS), Gastroesophageal Reflux Disease (GERD), and even serious illnesses like colorectal cancer.
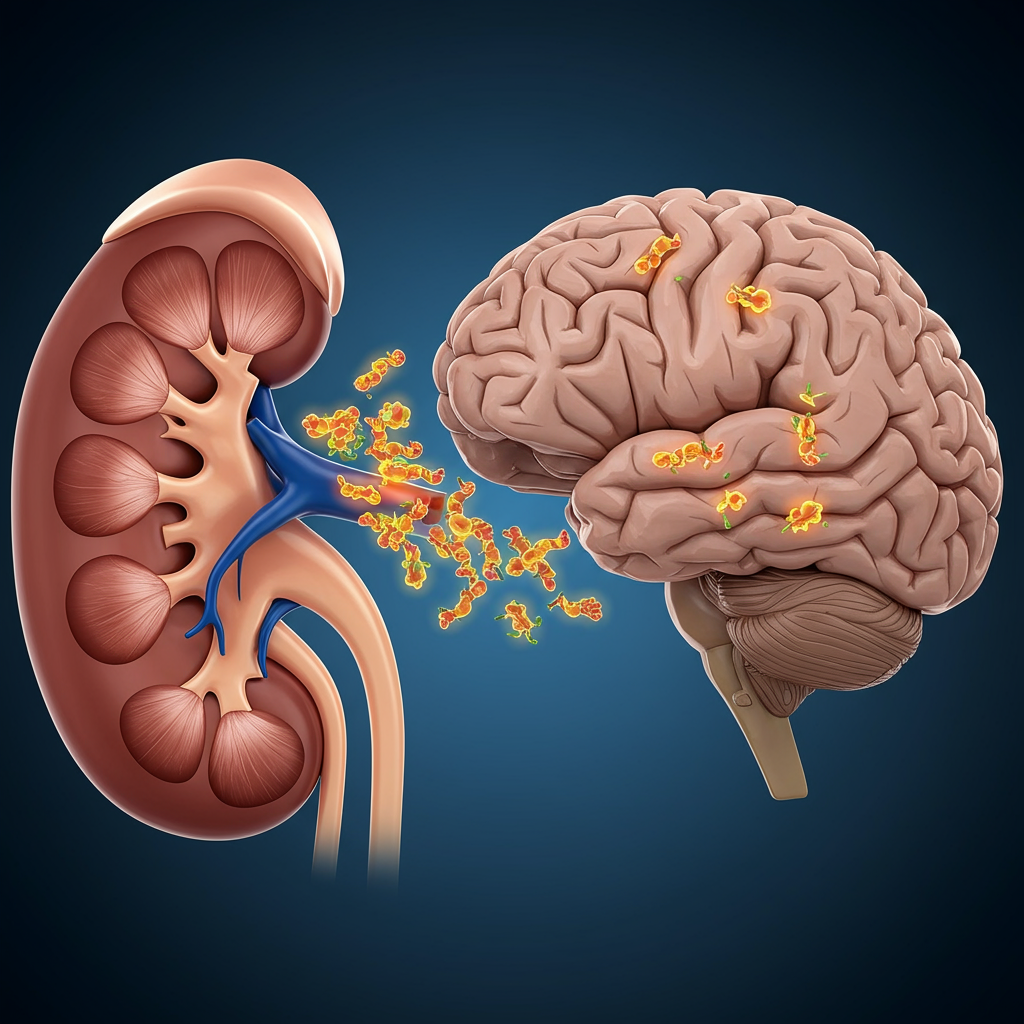
The connection between digestive health and other major medical conditions is well-established. Poor gut health has been linked to chronic diseases such as diabetes, heart disease, autoimmune disorders, and even neurological conditions like Alzheimer’s disease. Despite these connections and the sheer prevalence of symptoms, many individuals experiencing digestive distress do not seek professional medical care. This reluctance can lead to delayed diagnosis and treatment for potentially serious underlying conditions, highlighting a significant public health challenge.
Why Are Digestive Issues Becoming More Common in the US?
The reasons behind the apparent surge in digestive complaints are complex and likely stem from a combination of factors rooted in modern industrialized lifestyles. Our daily habits and environment play a crucial role in gut function.
One major contributor is undoubtedly diet. The typical modern diet often lacks sufficient fiber from fruits, vegetables, and whole grains, while being high in processed foods, sugar, and unhealthy fats. Inadequate physical exercise and insufficient fluid intake, particularly water, also negatively impact digestive motility and overall gut health. Rising rates of obesity, a condition closely tied to these lifestyle factors, are also associated with a higher risk of various digestive disorders.
Beyond lifestyle, mental health also significantly influences the gut. Increased levels of stress and anxiety, exacerbated by recent global events like the COVID-19 pandemic, are known to affect the digestive system. The gut-brain axis is a powerful connection, and psychological distress can manifest as physical symptoms, worsening conditions like IBS or contributing to others.
Furthermore, some research points to a potential direct link between COVID-19 infection and chronic gastrointestinal issues. A study conducted in 2022 found that a notable 29% of surveyed COVID-19 survivors reported experiencing at least one new chronic GI symptom as long as six months after their initial infection, suggesting a lasting impact of the virus on digestive health.
Most Common Digestive Reasons for Emergency Care (2018 Data)
While many digestive issues are managed at home or through outpatient care, some symptoms become severe enough to warrant an emergency department (ED) visit. Analyzing data from the Healthcare Cost and Utilization Project Nationwide Emergency Department Sample in 2018 provides insight into the digestive problems most frequently leading Americans to seek urgent hospital care. This data highlights the critical nature that common-sounding symptoms can sometimes take.
These five conditions represented the highest volume of digestive-related emergency department visits in the United States during that year:
Abdominal Pain
Ranking as the leading digestive complaint in EDs, abdominal pain accounted for a staggering 5.8 million annual visits, equivalent to 1,762 visits per 100,000 people. Abdominal pain is incredibly common and can originate from various organs within the abdomen or even from issues outside the digestive system. While often attributed to benign causes like gas, indigestion, or constipation, the rising prevalence of conditions such as food allergies, IBS, and GERD may be contributing to an increase in acute or severe cases requiring emergency evaluation. Persistent or severe abdominal pain should always be medically assessed.
Nausea and Vomiting
These unpleasant symptoms collectively represented the second most frequent digestive reason for ED visits, totaling 2.2 million annually, or 661 visits per 100,000 people. Nausea is the uncomfortable sensation that often precedes vomiting, the forceful expulsion of stomach contents. Both are non-specific symptoms that can indicate a vast array of underlying conditions, from minor infections to serious illnesses. Their potential increase may be linked to the rising rates of common triggers like stress, migraine headaches, food allergies, and the use of illicit drugs or excessive alcohol.
Noninfectious Gastroenteritis and Colitis
This condition, characterized by inflammation of the lining of the stomach and intestines, led to 1.3 million ED visits per year, or 386 per 100,000 people. Crucially, this classification refers to inflammation not caused by infectious agents like viruses or bacteria. Symptoms typically include nausea, vomiting, abdominal pain, and diarrhea. A potential rise in this condition may be associated with factors such as increased intentional or unintentional exposure to toxins – poison control calls saw a sharp rise between 2007 and 2021 – and potentially the increased or inappropriate use of medications known to irritate the GI tract, such as certain laxatives and antibiotics.
Constipation
Difficulty passing stools or having infrequent bowel movements, known as constipation, resulted in 1.1 million annual ED visits, or 332 per 100,000 people. This condition is experiencing a rapid increase in global cases, driven by several modern lifestyle factors. Dehydration is a major culprit, with nearly half of Americans reportedly not drinking enough water daily. Insufficient intake of dietary fiber is another significant factor, as only a small percentage of Americans consume the recommended amounts. Lack of physical activity also slows gut motility. Furthermore, the rising prevalence of associated chronic diseases like diabetes and IBS contributes to higher rates of constipation.
Gastrointestinal Bleeding
Ranking as the fifth most common digestive reason for emergency visits, GI bleeding accounted for 941,658 annual visits, approximately 288 per 100,000 people. This refers to any bleeding occurring in the digestive tract, from the esophagus to the rectum. Symptoms can range from visible blood in stool or vomit to subtle signs like paleness, weakness, and fatigue caused by blood loss. Severe bleeding can cause dramatic symptoms like dizziness or fainting. An increase in GI bleeding may be linked to the rising global incidence of cancers affecting digestive organs and the growing prevalence of Inflammatory Bowel Diseases (IBD) like Crohn’s disease and ulcerative colitis, which researchers suspect may be partly tied to diets high in processed foods and meat.
Don’t Ignore Your Symptoms: When to See a Doctor
Given the increasing trend of digestive issues and the potential for symptoms to signal serious conditions, it is paramount not to ignore persistent or worsening problems. While some digestive discomfort is temporary, the common reasons for emergency visits highlighted by the 2018 data underscore that these issues can become critical.
Self-diagnosis based on internet searches can be misleading and delay necessary medical intervention. If you experience new or significantly worsening digestive symptoms, especially severe pain, persistent vomiting, bloody stools, unexplained weight loss, or difficulty swallowing, it is crucial to consult a medical professional promptly. A doctor can properly evaluate your symptoms, determine the underlying cause, and recommend appropriate treatment, ensuring you receive the care needed to protect your health.
Frequently Asked Questions
Why are digestive issues becoming more common in the US?
Digestive problems are on the rise due to a combination of factors tied to modern lifestyles. These include poor diet low in fiber and high in processed foods, insufficient physical activity, and inadequate hydration. Increased stress and anxiety also play a role due to the gut-brain connection. Additionally, some research indicates a potential link between COVID-19 infection and new chronic digestive symptoms.
Where does the data on the most common digestive emergency visits come from?
The data highlighting the top five digestive reasons Americans visit the emergency department is based on analysis from the 2018 Healthcare Cost and Utilization Project Nationwide Emergency Department Sample. This comprehensive dataset provides insights into the most frequent severe digestive issues requiring urgent hospital care in the United States.
When should I be concerned about digestive symptoms and see a doctor?
You should consult a medical professional for any new or significantly worsening digestive symptoms. While mild, temporary issues can occur, persistent or severe symptoms like intense abdominal pain, frequent vomiting, blood in stool or vomit, unexplained weight loss, or difficulty swallowing warrant prompt medical evaluation. Do not rely on self-diagnosis.