<a href="https://news.quantosei.com/2025/07/04/structured-exercise-significantly-improves-survival-in-colon-cancer-patients-study-finds/” title=”Proven: Exercise Improves Colon Cancer Outcomes”>prostate cancer represents a significant health concern for men globally. While diagnoses and fatalities continue to rise, understanding the disease, its risks, and how to take proactive steps can make a vital difference. Early detection often leads to better outcomes and a higher chance of successful treatment. This guide delves into the essentials of prostate cancer, from understanding its nature to identifying risk factors and adopting healthy habits that may help reduce your risk.
What is Prostate Cancer?
Prostate cancer develops in the prostate gland, a small, walnut-sized organ exclusive to the male reproductive system. Located just below the bladder and in front of the rectum, the prostate plays a key role in producing seminal fluid, which nourishes and transports sperm. Cancer begins when cells within the prostate gland start to grow and multiply abnormally and uncontrollably. These malignant cells can form a tumor and, over time, may spread to other parts of the body if not detected and treated early.
Globally, prostate cancer is a leading cancer diagnosis among men. Projections for the United States in 2025 estimate hundreds of thousands of new cases, highlighting its prevalence.
Understanding Prostate Cancer Stages
Doctors classify prostate cancer into stages to describe how much cancer is in the body and where it is located. This staging is crucial for determining the best course of treatment and understanding the prognosis. A commonly used system is the AJCC (American Joint Committee on Cancer) TNM system.
Early Stage (Stages I & II)
Also known as localized prostate cancer, this means the cancer is confined entirely within the prostate gland. It hasn’t spread to the edges of the prostate or to nearby tissues. Early-stage cancer is typically more treatable and has a better prognosis compared to later stages.
Locally Advanced Stage (Stage III)
In this stage, the cancer has grown beyond the prostate gland. It may have invaded nearby tissues, such as the seminal vesicles (glands that produce fluid that mixes with sperm). However, it has not yet spread to distant lymph nodes or organs.
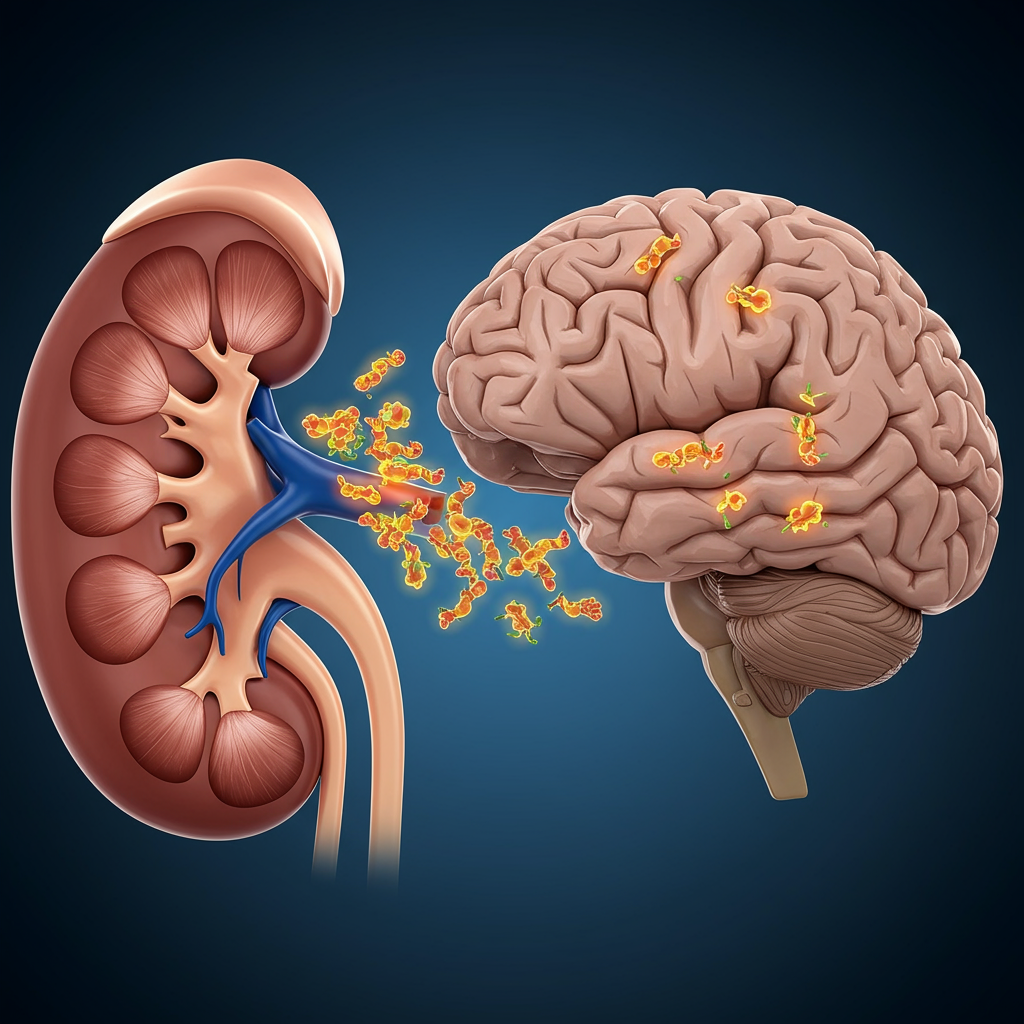
Advanced or Metastatic Stage (Stage IV)
This is the most serious stage, where the cancer has spread (metastasized) from the prostate to distant parts of the body. Common sites for metastasis include bones, distant lymph nodes, liver, and lungs. Advanced prostate cancer is more challenging to treat and often focuses on managing the disease and its symptoms.
Recognizing Prostate Cancer Symptoms
A key challenge with prostate cancer is that in its early stages, it frequently causes no noticeable symptoms. This lack of early warning signs underscores the importance of regular health check-ups and understanding your personal risk factors.
Potential Symptoms When Present
When symptoms do appear, they often relate to the prostate’s proximity to the bladder and urethra or indicate more advanced disease. Look out for:
Difficulty starting urination or a weak or interrupted flow.
Frequent urination, especially at night.
Pain or a burning sensation during urination.
Blood in the urine or semen.
Erectile dysfunction (difficulty getting or keeping an erection).
Painful ejaculation.
Dull pain or discomfort in the lower pelvic area.
Bone pain (often in the back, hips, or thighs), which can signal the cancer has spread.
Loss of appetite or unexplained weight loss.
Experiencing these symptoms doesn’t automatically mean you have prostate cancer, as other non-cancerous conditions can cause similar issues. However, it is essential to see a doctor for proper evaluation if any of these symptoms arise.
Key Risk Factors for Prostate Cancer
While the precise cause of prostate cancer is not fully understood, several factors are known to increase a man’s risk of developing the disease.
Age is a Primary Factor
The risk of prostate cancer increases significantly with age. It is most commonly diagnosed in men over 50. Part of this increased risk in older men is associated with the natural enlargement of the prostate gland over time, although the reasons are complex.
Family History Plays a Major Role
Having a father or brother who has had prostate cancer more than doubles a man’s risk. The risk is higher if the affected relative was diagnosed at a younger age or if multiple family members have had the disease. Sharing your family health history with your doctor is crucial.
Genetic Factors and Inherited Mutations
Certain inherited gene mutations can increase risk. Mutations in genes like BRCA1 and BRCA2, commonly associated with breast and ovarian cancers, also elevate a man’s prostate cancer risk. More recent research highlights the role of a Polygenic Risk Score (PRS). This score, which looks at multiple gene variants linked to prostate cancer, can identify men with a significantly higher genetic predisposition. Studies indicate men with a PRS in the top 10% face a 40-50% lifetime chance of diagnosis.
Race and Ethnicity
Research shows that African American men have a higher risk of developing prostate cancer and are more likely to develop aggressive forms of the disease compared to white men. The reasons for this disparity are complex and involve genetic, environmental, and socioeconomic factors.
Obesity
Being overweight or obese is linked to a higher risk of developing more aggressive forms of prostate cancer. It is also associated with a greater likelihood of the cancer recurring after initial treatment.
Smoking
Observational studies suggest that while smoking might not strongly influence the incidence of prostate cancer, it is associated with a higher risk of recurrence and metastasis (spread) in men who are diagnosed. Quitting smoking offers numerous health benefits, including potentially better outcomes if prostate cancer is diagnosed.
Diagnosing Prostate Cancer
Detecting prostate cancer early, often before symptoms appear, is key to improving treatment success rates. Several tests can help diagnose the disease.
Digital Rectal Exam (DRE)
During a DRE, a doctor manually checks the prostate gland for any abnormalities in size, shape, or texture by inserting a gloved, lubricated finger into the rectum. This can sometimes detect tumors on the back of the prostate.
Prostate-Specific Antigen (PSA) Test
The PSA test is a blood test that measures the level of prostate-specific antigen, a protein produced by the prostate gland. Elevated PSA levels can indicate various prostate issues, including cancer, but also non-cancerous conditions like benign prostatic hyperplasia (BPH) or prostatitis. A doctor will interpret PSA levels in conjunction with other factors, including age and DRE findings.
Imaging Tests
If the PSA is high or the DRE is abnormal, imaging tests may be used. Magnetic Resonance Imaging (MRI) is increasingly common to help visualize the prostate and identify suspicious areas before a biopsy.
Prostate Biopsy
If initial tests suggest cancer, a prostate biopsy is usually performed. This involves taking small tissue samples from the prostate using a needle, often guided by ultrasound or MRI. A pathologist then examines the samples under a microscope to check for cancer cells. A biopsy is necessary to confirm a diagnosis of prostate cancer.
The Importance of Screening Discussions
For men aged 50 and older, particularly those with risk factors like a strong family history or African American ethnicity, discussing prostate cancer screening with a healthcare provider is recommended. This is often a shared decision-making process, weighing the potential benefits of early detection against the risks and potential side effects of treatment. Recent findings regarding genetic risk scores (PRS) may further inform who could benefit most from targeted or earlier screening. Remember, “early detection equals better outcomes,” leading to more treatment options and a higher chance of survival.
Healthy Habits for Prostate Health and Risk Reduction
While you cannot change your age, family history, or genetic makeup, several lifestyle modifications can significantly impact your overall health and may help reduce your risk of developing prostate cancer or developing a more aggressive form of the disease, especially for those with higher genetic risk.
Embrace a Healthy Diet
Eating a balanced, plant-based diet rich in fruits, vegetables, and whole grains is strongly recommended. Studies suggest consuming multiple servings of non-starchy vegetables and fruits daily is linked to a lower risk of death from cancer overall. Limit your intake of red and processed meats, saturated fats, and high-sugar foods. A diet low in processed meat and saturated fat while being high in fruits and vegetables is specifically highlighted as potentially beneficial for men with a higher genetic predisposition to prostate cancer.
Stay Physically Active
Regular exercise offers numerous health benefits, including potentially reducing the risk of certain cancers. Aim for at least 30 minutes of moderate-intensity physical activity five or more days a week. This could include brisk walking, jogging, swimming, or other activities that make you breathe faster and sweat lightly. Maintaining a healthy weight through diet and exercise is crucial, as obesity is a known risk factor for aggressive prostate cancer.
Maintain a Healthy Weight
Being overweight or obese is associated with an increased risk of more aggressive prostate cancer. Working towards and maintaining a healthy body weight through diet and exercise can be a protective measure.
Avoid Tobacco Use
Smoking is linked to many cancers and can worsen outcomes for men with prostate cancer. If you smoke, quitting is one of the single most important steps you can take for your health. It’s never too late to stop, and the benefits begin immediately.
Limit Alcohol Consumption
Higher alcohol intake is associated with an increased risk of several cancers. If you drink alcohol, do so in moderation – generally defined as no more than two drinks per day for men.
Understand Your Genetic Risk
While PRS testing is still evolving in clinical practice, being aware of your family history and discussing genetic testing options with your doctor, especially if you have a strong family history of prostate or other related cancers (like breast or ovarian), can provide valuable insight into your personal risk profile. For those identified with higher genetic risk, adopting a healthy lifestyle becomes even more critical for potentially mitigating mortality risk, as roughly one-third of early deaths in this group might be preventable through behavioral changes.
Adopting these healthy habits isn’t a guarantee against prostate cancer, but it empowers you to take control of factors you can influence. Combined with regular check-ups and informed discussions about screening with your doctor, these steps contribute to a comprehensive approach to men’s health.
Frequently Asked Questions
What is prostate cancer and who is most at risk?
Prostate cancer is a disease where cells in the prostate gland grow abnormally. The prostate is a small gland below the bladder in men. The primary risk factors include age (risk increases significantly after 50), family history (having a father or brother with the disease, especially if diagnosed young), and genetics (certain mutations and a higher polygenic risk score or PRS). African American men also face a higher risk.
Can lifestyle changes like diet and exercise really prevent prostate cancer?
While lifestyle changes don’t offer a guarantee of prevention, they are strongly associated with a reduced risk of developing aggressive prostate cancer and, importantly, reducing the risk of dying* from the disease. Research suggests that for men with a high genetic risk (high PRS), adopting healthy habits like maintaining a healthy weight, exercising regularly, eating a plant-based diet, and avoiding smoking could potentially prevent a significant percentage of early prostate cancer deaths. These habits are a powerful way to mitigate risk, especially if you are predisposed.
When should men talk to their doctor about prostate cancer screening?
Discussion about prostate cancer screening is generally recommended for men starting around age 50. However, if you have known risk factors such as a strong family history of prostate cancer (especially in close relatives diagnosed before age 65) or are an African American man, these discussions should begin earlier, often around age 40 or 45. It’s a personalized decision that should be made in collaboration with your doctor after considering your individual risk factors and health status.
Living a healthy lifestyle and being proactive about your health are essential steps. Discussing your personal risk factors and appropriate screening schedules with your healthcare provider is the best way to stay informed and empowered regarding prostate cancer.