Facing a cancer diagnosis and undergoing <a href="https://news.quantosei.com/2025/07/01/landmark-dna-study-charts-blood-ageing-caused-by-cancer-drugs/” title=”Essential DNA Study Links Cancer Drugs to Blood Aging”>chemotherapy is a life-saving battle for millions. While incredibly effective at destroying cancer cells, these powerful treatments can have lasting effects on the body, some of which scientists are just beginning to understand. A critical area of focus is how chemotherapy impacts normal, healthy cells, particularly the blood-producing cells that are essential for life.
Breakthrough research, spearheaded by experts at MD Anderson Cancer Center, is uncovering a hidden cost: chemotherapy drives profound genetic and structural changes in blood stem cells. These alterations may significantly increase the risk of developing secondary blood cancers, often many years or even decades after successful treatment of the initial malignancy. Understanding this risk is a crucial step toward developing strategies to prevent these devastating late complications.
The Foundation: Understanding Blood Stem Cells
Our bodies rely on a continuous supply of fresh blood cells – red cells, white cells, and platelets. These cells originate from a special population of cells found primarily in the bone marrow: Hematopoietic Stem and Progenitor Cells, or HSPCs.
HSPCs are remarkable. They possess the unique ability to both self-renew (make more of themselves) and differentiate (turn into all the different types of mature blood cells). This longevity and regenerative capacity make them vital, but also vulnerable. Over a lifetime, as HSPCs divide, they can accumulate random DNA mutations. This natural process contributes to aging and is the basis of conditions like clonal hematopoiesis, where clones of cells with certain mutations expand.
Uncovering Chemotherapy’s Deep Impact
Scientists have long known that chemotherapy can increase the risk of secondary malignancies, particularly myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML), collectively known as therapy-related myeloid neoplasms (t-MNs). What wasn’t fully clear was the precise biological mechanism by which chemotherapy induces this risk within normal HSPCs.
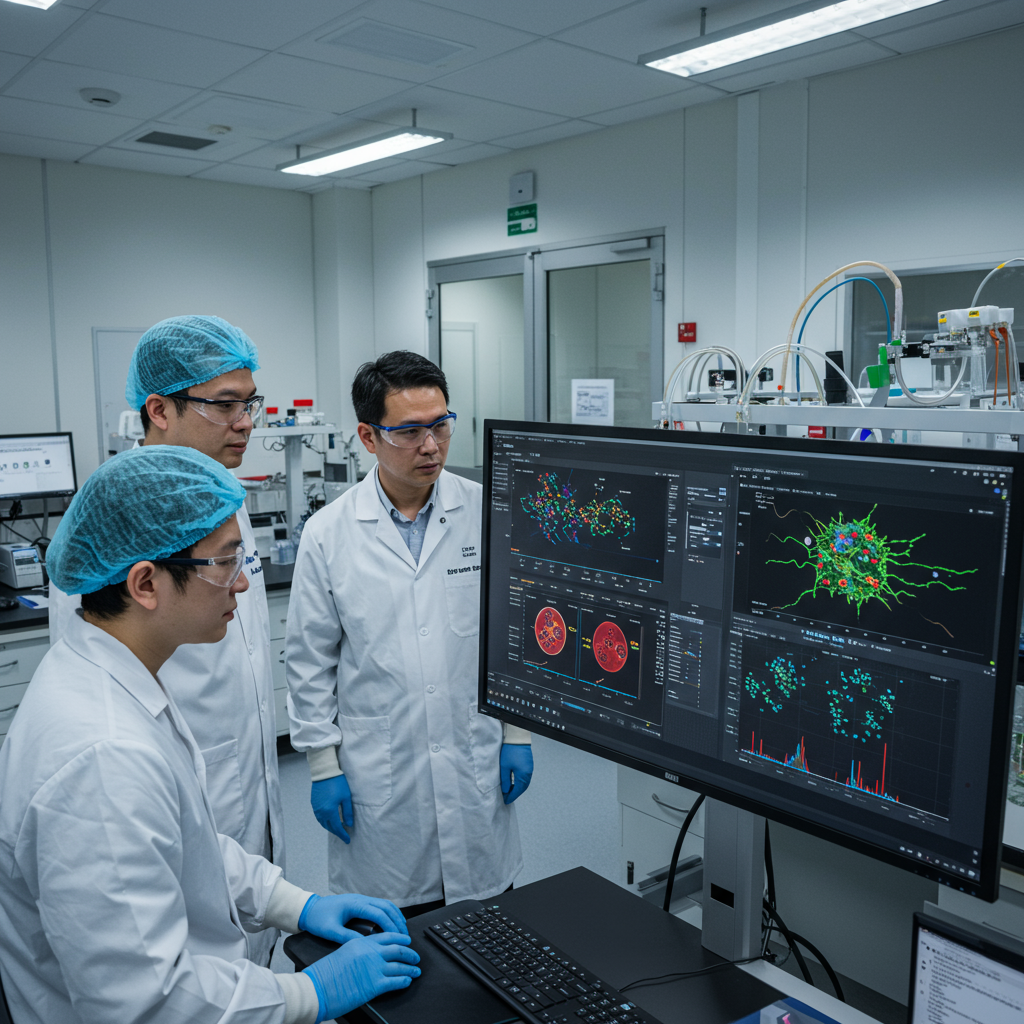
To investigate this, a comprehensive study led by Koichi Takahashi, M.D., Ph.D., involved detailed genetic analysis of blood cells. Researchers analyzed samples from 23 individuals who had received various chemotherapy treatments for different cancers. They compared these findings to samples from 9 healthy individuals who had not been exposed to chemotherapy.
Using advanced techniques like whole-genome sequencing of single HSPCs and sophisticated analysis of mature blood cell types, the team could map out the genetic changes occurring in these vital cells. This allowed them to see the full picture of chemotherapy’s effect on both individual cell mutations and the overall population structure of blood-forming cells.
Key Finding 1: Chemotherapy Leaves a Distinct Mutational Mark
The study revealed a striking result: chemotherapy significantly increases the total number of mutations in normal blood cells. In many treated individuals, mutation levels were far higher than expected based on their age alone. This means chemo isn’t just affecting cancer cells; it’s causing widespread genetic damage in healthy blood stem cells as well.
Even more revealing was the discovery of specific “mutational signatures.” Different chemotherapy drugs leave distinct fingerprints on the DNA. For example, the study identified unique patterns of DNA damage associated with drugs like melphalan, chlorambucil, bendamustine, procarbazine, platinum agents (like cisplatin and carboplatin), and 5-fluorouracil (5-FU).
This finding is crucial. It shows that not all chemotherapy drugs have the same mutagenic effect on normal blood cells. Even within the same drug class, agents used interchangeably in the clinic can have vastly different impacts at the genomic level. The effects also varied depending on the specific type of blood cell examined (stem cells vs. different mature immune cells).
Key Finding 2: Accelerated Clonal Aging
Beyond just increasing the overall mutation burden, chemotherapy profoundly alters the way blood stem cell populations evolve over time. Normally, as people age, specific clones of HSPCs carrying mutations in genes like DNMT3A or TET2 can expand. This is a natural process called clonal hematopoiesis (CH).
However, the study found that chemotherapy exposure accelerates a similar process, but with a critical difference. Instead of primarily selecting for DNMT3A or TET2 mutations, chemotherapy appears to strongly select for clones with mutations in DNA repair and response genes, such as PPM1D and TP53.
These mutant clones gain a survival advantage in the harsh environment created by chemotherapy. They expand prematurely, leading to an “aged” clonal architecture in blood stem cells years or even decades earlier than would typically occur. This creates a population heavily populated by these specific “high-risk” clones.
Connecting the Dots: From Stem Cell Changes to Secondary Cancer Risk
The findings paint a clear picture of how chemotherapy increases the risk of secondary blood cancers. The increased overall mutation load in HSPCs provides a larger pool of cells that could acquire additional, “second hit” mutations necessary for full malignant transformation, such as mutations in proliferation signaling genes.
Simultaneously, the chemotherapy-driven selection and expansion of high-risk clones, particularly those with PPM1D and TP53 mutations, create a large reservoir of preleukemic cells. These clones are already genetically unstable or primed to survive damage. They are more susceptible to acquiring those subsequent mutations that drive the cells down a path toward leukemia or MDS. This explains why secondary blood cancers can emerge many years after the initial treatment.
Dr. Koichi Takahashi highlighted the significance, stating that the research “uncovers the hidden long-term effects of chemotherapy on normal hematopoietic stem cells, revealing accelerated clonal aging and the emergence of high-risk hematopoietic clones that predispose to leukemic transformation.”
Implications for Patients and Clinical Care
This groundbreaking research has important clinical implications:
Improved Risk Assessment: Understanding which chemotherapy regimens and specific drugs are most mutagenic to normal HSPCs could help clinicians better assess an individual patient’s long-term risk of developing t-MNs.
Potential for Early Detection: Identifying the specific high-risk clones (like those with PPM1D or TP53 mutations) that emerge and expand years after treatment could potentially lead to early detection strategies. Monitoring for these clones in long-term survivors might allow for intervention before overt leukemia develops.
Treatment Optimization: Knowing the differential effects of various chemotherapy agents on normal stem cells might inform future treatment protocols. For example, if multiple drug options exist for a primary cancer, choosing an agent with a lower mutagenic signature on HSPCs could potentially reduce the risk of secondary cancers without compromising efficacy against the primary tumor. Research into this area is ongoing.
Stem Cell Transplant Screening: For patients undergoing stem cell transplantation, understanding clonal changes in donor or recipient cells could be increasingly important. (Internal link opportunity: Learn more about stem cell transplantation).
The study suggests that the premature shift in clonal architecture driven by chemotherapy, featuring the expansion of PPM1D and TP53 mutant clones, is a plausible major contributor to long-term complications including secondary hematological malignancies and impaired bone marrow function.
Frequently Asked Questions
What kind of blood stem cells are affected by chemotherapy?
Chemotherapy primarily affects hematopoietic stem and progenitor cells (HSPCs). These are the master cells in the bone marrow that produce all types of mature blood cells, including red blood cells, white blood cells, and platelets. Because they are long-lived and constantly dividing, they are particularly susceptible to DNA damage and the accumulation of mutations caused by chemotherapy agents.
Which chemotherapy drugs are mentioned as potentially increasing mutation risks in this study?
The study found that various chemotherapy drugs leave specific mutational fingerprints on normal blood stem cells. Drugs highlighted as having significant mutagenic impacts or distinct signatures included melphalan, chlorambucil, bendamustine, procarbazine, platinum agents (like cisplatin and carboplatin), and 5-fluorouracil (5-FU) or capecitabine. The study showed mutagenic effects varied even among drugs within the same class.
How does chemotherapy increase the risk of secondary blood cancers decades later?
Chemotherapy increases this risk in two main ways according to the research. First, it increases the overall number of DNA mutations in blood stem cells. Second, it accelerates a process similar to aging by selecting for and causing the premature expansion of specific clones of stem cells that have acquired mutations in genes like PPM1D and TP53. These expanded, high-risk clones are more prone to acquiring further mutations over time, eventually leading to the development of therapy-related myeloid neoplasms (leukemia or MDS) many years after the initial treatment.
A Future Focused on Prevention
This detailed research into the long-term genomic consequences of chemotherapy on normal blood stem cells is a significant step forward. It moves beyond simply acknowledging the risk of secondary cancers to explaining the underlying biological mechanisms. By pinpointing the specific genetic changes and clonal expansions involved, scientists and clinicians are better equipped to identify individuals at higher risk, explore preventative strategies, and potentially refine treatment approaches to minimize long-term damage to vital blood-forming cells. Continued research is essential to translate these findings into tangible benefits for cancer survivors worldwide. (Internal link opportunity: Explore other research highlights from MD Anderson).